Vasectomy represents a surgical procedure for male sterilization and is considered the most reliable form of male contraception. During this procedure, the vas deferens tubes that connect the testes with the urethra are divided and subsequently occluded in order to prevent spermatozoa entering into the semen.
In one form or another, this procedure has been performed for over 100 years, but the main advance in male sterilization was seen in 1974 in China with the rise of non-scalpel vasectomy. Following its success, this technique was eventually introduced in 1985 in the United States, and in 1995 in the United Kingdom.
Unlike other areas of minor surgery (where the proper patient care includes clinical appraisal, presumptive diagnosis and surgery), in vasectomy the patient undertakes his own assessment and diagnosis. Therefore it is pivotal that the specialist offering this service provides comprehensive counselling to fully inform the patient.
Indications, contraindications and practical considerations
Motivations for having a vasectomy differ, thus the decision has to be made in a situation without any compulsion or stress. In general, vasectomy is indicated for any fully informed man who does not want to father any children and who desires an inexpensive outpatient method of voluntary permanent surgical sterilization. It must be stressed that the respect for the patient’s personal decision is essential.
Naturally, there are no absolute contraindications, but younger age (less than 30 years), the absence of children, no current relationship, certain severe illnesses and scrotal pain can be considered as relative contraindications. Specific anatomic abnormalities, large varicoceles and hydroceles, as well as acute skin infections are also considered contraindications for this procedure.
Extreme consideration has to be taken with patients who are on anticoagulant or antiplatelet medications. Moreover, alternative methods of birth control, possible surgical complications and failure rates should be thoroughly discussed. Needless to say that emotional instability and equivocal feelings about permanent sterilization must be addressed, and a written informed consent is recommended.
Vasectomy methods
In general, this procedure can be performed as an open vasectomy, or as a non-scalpel vasectomy using fine sharp instruments to puncture the skin and deliver the vas for ligature, i.e. excising a segment of vas and repositioning the ends of the vas either with or without ligation (with the latter known as open-ended vasectomy).
Vasectomy can be done in an outpatient setting using local anesthesia, while general anesthesia is required for specific indications. Techniques that can be applied for discontinuation of the deferential ducts are interposition of tissue (preventing recanalization), excision of a piece of vas deferens and its subsequent ligation, as well as cautery of the luminal side.
Mutual comparison of different methods has not shown convincing superiority of one particular approach in terms of preventing pregnancy. Still, post-vasectomy semen analysis has shown that the occlusion failure is the highest in methods with simple excision and ligation with sutures or clips, whereas techniques combining fascial interposition and cautery have the lowest failure rate.
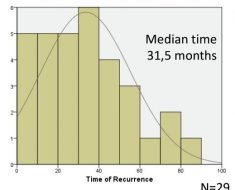
Following a short recovery period, more than 80% of patients return to normal activities within one week. An indispensable part of the follow-up is semen analysis, which is ideally performed three months after the procedure in a certified laboratory. Men can be given clearance if no spermatozoa are observed in the ejaculate.
Sources
- http://www.aafp.org/afp/1999/0701/p137.html
- http://www.aafp.org/afp/2006/1215/p2069.html
- www.vasectomie.net/…abrecque_%20vasectomyocclusiontechnique_2009.pdf
- uroweb.org/…/…rol-Esp-2012-365276.-EAU-guidelines-on-vasectomy.pdf
- Kabir A. Vasectomy: No Scalpel Method. In: Salam MA, editor. Principles and Practice of Urology, Second Edition, Volume One. Jaypee Brothers Medical Publishers (P) LTD, 2013; pp. 705-708.
- Spooner L, Feltbower T. Vasectomy: knowledge. In: Botting J, Schofield J, editors. Brown's Skin and Minor Surgery: A Text and Colour Atlas, Fifth Edition. CRC Press, Taylor & Francis Group, LLC, 2015; pp. 161-168.
Further Reading
- All Vasectomy Content
- Vasectomy Side Effects
- Vasectomy Complications
- Vasectomy Reversal
Last Updated: Aug 23, 2018

Written by
Dr. Tomislav Meštrović
Dr. Tomislav Meštrović is a medical doctor (MD) with a Ph.D. in biomedical and health sciences, specialist in the field of clinical microbiology, and an Assistant Professor at Croatia's youngest university – University North. In addition to his interest in clinical, research and lecturing activities, his immense passion for medical writing and scientific communication goes back to his student days. He enjoys contributing back to the community. In his spare time, Tomislav is a movie buff and an avid traveler.
Source: Read Full Article