Mononeuritis multiplex occurs when there is damage to two or more distinct nerve areas. It can also be known as mononeuropathy multiplex or multiplex neuropathy and is defined as a combination of symptoms rather than a disease in its own right.
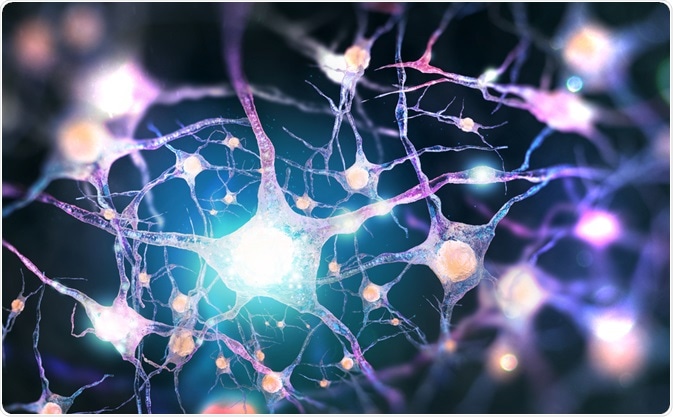
Image Credit: Andrii Vodolazhskyi/Shutterstock.com
What symptoms comprise mononeuritis multiplex?
The Mononeuritis complex covers many different types of nerve damage that can occur to the peripheral nervous system. It is characterized by dysfunction of several nerve areas that are distinct from one another, unlike in polyneuropathy where the dysfunction occurs more locally.
Most symptoms are related to the sense of touch. This includes feelings of numbness, tingling, and weird sensations or no sensations at all. Other symptoms relate more to overall mobility. Some of the more common symptoms include not being able to control the body’s movement or losing the ability to move parts of the body. Mononeuritis multiplex is usually only acute or subacute but can in rare cases be chronic.
Causes and risk factors of mononeuritis multiplex
Mononeuritis multiplex can affect anyone but is more common in people with certain conditions. However, while these conditions may cause mononeuritis multiplex to occur, they can be mild conditions and are not always identified. Previously, the underlying cause could not be identified in around half of all cases of mononeuritis multiplex, but this has been improved in recent decades.
The conditions that can cause mononeuritis multiplex include diabetes mellitus, diseases of the connective tissues, and vasculitis. Of these, vasculitis is the most common cause of mononeuritis multiplex. Another common cause is diabetes mellitus and oxygen deprivation as a result of low blood flow to certain areas, which can cause cellular death.
Vasculitis is characterized by inflammation surrounding the blood vessels, which can in turn affect the arteries surrounding the peripheral nerves or blood vessels around certain nerves. This can occur in several different disorders, such as rheumatoid arthritis, scleroderma, and systemic lupus erythematosus.
Apart from diabetes mellitus and nerve compressions, rheumatoid arthritis is a common cause. Some studies have shown that as many as 56% of patients with mononeuritis multiplex, who do not have diabetes or nerve compression, have rheumatoid arthritis as the underlying condition causing the symptoms. For many of these, the arthritis was not previously diagnosed and had occurred recently.
Other causes of mononeuritis multiplex include extreme allergic reactions to drugs or violent reactions to infections. In rare cases, mononeuritis multiplex can be caused by bacterial or viral infection directly in the nerves. For example, mononeuritis multiplex can be linked to HIV infections and hepatitis B infections. Cancer can also cause mononeuritis multiplex, especially if a tumor is interfering with a nerve.
Due to the nature of the conditions that can cause mononeuritis multiplex, certain risk factors increase the chance of being afflicted with the condition. For example, while old age is a general risk factor for diabetes mellitus, those with diabetes who develop mononeuritis multiplex tend to be elderly and have mild or undiagnosed diabetes. Similarly, only around one-third of those afflicted with mononeuritis multiplex have been diagnosed with the underlying condition before the onset of symptoms of mononeuritis multiplex.

Image Credit: Douglas Olivares/Shutterstock.com
Diagnosis and treatment
Diagnosis is often made in connection with any of the above conditions that underlie the occurrence of mononeuritis multiplex. Diagnosis can be done in conjunction with nerve conduction velocity tests and electromyogram. Alternatively, a nerve biopsy can be taken. Nerves afflicted with mononeuritis multiplex have certain characteristics that are detectable through biopsies – notably, there tends to be a degree of dead tissue in the peripheral nerve trunks.
Treatment for mononeuritis multiplex is difficult since it can be triggered by so many underlying conditions. While therapy aims to get the symptoms of mononeuritis multiplex under control, full recovery is possible if the underlying cause can be identified and treated.
For the most common cause of mononeuritis multiplex, vasculitis, and other neuropathies of the vasculature, treatment is most commonly done with methylprednisolone administered intravenously, corticosteroids administered orally, and cyclophosphamide administered orally.
Orally administered cyclophosphamide and azathioprine can be used when mononeuritis multiplex is chronic. In some other forms of mononeuritis multiplex, exchanging the plasma and administering immune globulin intravenously may be an effective treatment method.
Sources
- American Association of Neuromuscular & Electrodiagnostic Medicine. 2020. Mononeuritis Multiplex. [online] Available at: <https://www.aanem.org/Patients/Muscle-and-Nerve-Disorders/Mononeuritis-Multiplex#:~:text=Mononeuritis%20multiplex%2C%20also%20known%20as,rather%20than%20its%20own%20disease.> [Accessed 15 September 2020].
- Scott, K., and Kothari, M., 2019. Mononeuritis Multiplex – Symptoms, Diagnosis, and Treatment. [online] British Medical Journal Best Practice. Available at: <https://bestpractice.bmj.com/topics/en-us/799> [Accessed 15 September 2020].
- Raff, M., Sangalang, V., and Asbury, A., 1968. Ischemic Mononeuropathy Multiplex Associated with Diabetes Mellitus. Archives of Neurology, 18(5), pp. 487-499.
- Hellmann, D., Laing, T., Petri, M., Whiting-OʼKeefe, Q. and Parry, G., 1988. Mononeuritis Multiplex: the yield of evaluations for occult rheumatic diseases. Medicine, 67(3), pp. 145-153.
Last Updated: Sep 16, 2020

Written by
Sara Ryding
Sara is a passionate life sciences writer who specializes in zoology and ornithology. She is currently completing a Ph.D. at Deakin University in Australia which focuses on how the beaks of birds change with global warming.
Source: Read Full Article