In Canada, around 230,000 people are currently infected with hepatitis B, and a further 250,000 with hepatitis C.
Both hepatitis B and hepatitis C are serious liver infections which, if left untreated, can cause cirrhosis, liver cancer and early death.
In 2016, Canada was one of 194 nations globally to sign up to World Health Organisation (WHO) targets to eliminate both diseases by 2030. These targets require 90 per cent of children to have received the three doses of hepatitis B vaccination by 2030. They also entail a 90 per cent reduction in mother-to-child transmission of the virus.
This week, I will be chairing the Global Hepatitis Summit in Toronto (June 14-17). At this summit, we will be appealing for all Canadian children to be offered the hepatitis B vaccine, as currently recommended by WHO.
Right now, most provinces vaccinate children when they are much older, with some such as Ontario and Nova Scotia leaving it as late as 12 years old.
It is time we offered all children in Canada protection from hepatitis B from the moment they are born, as already happens in most developed countries —and also many developing countries.
Children at highest risk
Sexual activity is one of the ways hepatitis B can be transmitted. This has led to the misconception that we only need to offer older children vaccination, in the years before they become sexually active.
However, all babies and young children face other risks of blood to blood transmission —from the moment they are born. Hepatitis B can be transmitted at home, at school playing together with other children and in many other places.
Another problem is that in Canada we only vaccinate children at birth when we know the mother has hepatitis B —in order to prevent transmission at birth. This adds a lot of complexity to the system and is prone to errors. If the systems fails, children will be unnecessarily infected with this terrible virus at birth.
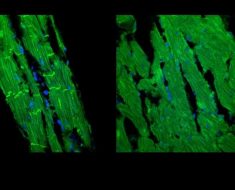
Hepatitis B also hits babies and young children much harder than adults. More than 90 per cent of those infected will develop a chronic hepatitis B infection. And chronic infections can, if left untreated, cause progression to liver cirrhosis, liver cancer and death.
While the risk of this progression is highest when infected under the age of one, up to 50 per cent of young children between one and five years who are infected will develop a chronic hepatitis B infection.
For anyone over 18, this risk is reduced to five to 10 per cent of those infected.

A vaccination lottery
WHO recommends that all infants should receive their first dose of vaccine as soon as possible after birth, preferably within 24 hours.
Yet Canada’s hepatitis B vaccination policy varies widely between provinces and territories. Most of the provinces with large populations vaccinate children when they are long past infancy: Manitoba at age nine years, Alberta at 10 years, Saskatchewan and Newfoundland and Labrador at age 11, and Ontario and Nova Scotia at 12.
British Columbia introduced vaccination for very young infants from age two months in 2001. Quebec did the same in 2013, although the province still vaccinates older children at nine years who are not covered by their new program.
Prince Edward Island and the Yukon also vaccinate young children from age two months, but it is only in New Brunswick, and the sparsely populated Nunavut and Northwest Territories, that all children are offered vaccination at birth.
Since all children across Canada will eventually be offered vaccination regardless of where they live, why don’t we just remove this lottery and routinely vaccinate them all from birth?
This is the best way to ensure that they are all vaccinated and none slip through the system. This will reduce new cases of hepatitis B among children to near zero and remove the chance that any of them will become chronically infected.
It is also much easier logistically to vaccinate children at birth. After the first dose, the two follow-up vaccinations can be combined with other routine vaccines given in the first year. And this protection will usually last a lifetime.
Prevention of cirrhosis and liver cancer
At the moment, hepatitis B infection is treatable, but not curable. For those on treatment, this is usually lifelong and helps prevent progression of liver damage to full blown cirrhosis and liver cancer.
Also at this week’s Global Hepatitis Summit, we will discuss a range of new therapies on the horizon to treat those people with the virus. But as with any disease, the best way to deal with it is prevention.
Source: Read Full Article