People with a higher risk of developing cardiovascular disease have increased cognitive decline, including an increase in typical markers of Alzheimer’s disease, suggesting that monitoring and controlling for heart disease may be key to maintaining and improving cognitive health later in life, according to research published today in the Journal of the American College of Cardiology.
Dementia is a public health challenge, with 50 million people affected in 2017 and the World Health Organization predicting 82 million people by 2030. There is not currently an effective treatment for dementia, so identifying modifiable risk factors that could delay or prevent dementia onset are becoming more prominent.
Previous studies have reported how cardiovascular disease risk factors were related to smaller volumes of specific brain regions, such as white matter, gray matter and hippocampus, but findings have been inconsistent. Researchers in this study sought to compare Framingham General Cardiovascular Risk Scores (FGCRS), which incorporate demographic information with traditional cardiovascular risk factors to assess future risk, to an individual’s long-term decline in global and domain specific cognitive function.
Researchers followed 1,588 dementia-free participants from the Rush Memory and Aging Project for 21 years. The average age was 79.5 years. Their FGCRS was assessed at baseline and categorized into lowest, middle and highest groups according to heart disease risk. Each year participants’ episodic memory (memory of everyday events), semantic memory (long-term memory), working memory (short-term memory), visuospatial ability (capacity to identify visual and spatial relationships among objects) and perceptual speed (ability to accurately and completely compare letters, numbers, objects, pictures or patterns) was assessed using 19 tests to derive a composite score.
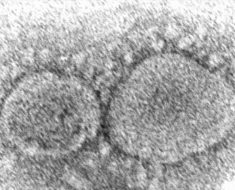
At the end of the study period, researchers found that having a higher cardiovascular risk burden was associated with faster decline in episodic memory, working memory and perceptual speed. Researchers also looked at MRI data for a subset of patients and found that higher FGCRS was associated with smaller volumes of hippocampus, cortical gray matter and total brain. Decreases in hippocampal and gray matter are typical markers of Alzheimer’s dementia-related neurodegeneration. MRIs also showed a greater volume of white matter hyperintensities, which are white spots on the brain that cause an area to decline in functionality.
Episodic memory and working memory were related to hippocampal volume, but perceptual speed was associated with white matter hyperintensities in the study, showing that results from the memory tests and the MRI were complementary.
“In the absence of effective treatments for dementia, we need to monitor and control cardiovascular risk burden as a way to maintain patient’s cognitive health as they age,” said Weili Xu, Ph.D., Department of Epidemiology and Biostatistics, School of Public Health, Tianjin Medical University, Tianjin, China. “Given the progressive increase in the number of dementia cases worldwide, our findings have both clinical and public health relevance.”
Study limitations include that participants were volunteers from the community, which could limit the generalizability of the findings, and that participants were generally well-educated and performed relatively well on cognitive tests, so the observed association may have been an underestimation.
In a related editorial comment, Costantino Iadecola, MD, Feil Family Brain and Mind Research Institute, Weill Cornell Medicine, New York, said exploring the use of a common cardiovascular risk score like FGCRS to assess cognitive decline is highly relevant.
Source: Read Full Article