New research has found measuring a protein that forms to create new blood vessels after a heart attack or unstable angina, and determining the protein’s genetics, could potentially help to predict long-term survival, specifically in heart patients.
The study, recently published in scientific journal PLOS ONE, has shown the presence or absence of a gene variant for the protein, can help predict the long-term survival chances in males, who have experienced an acute coronary event.
Massey University School of Health Sciences’ Dr. Barry Palmer says the human body’s ability to recover from severe health events like heart attacks, is helped by its capacity to form new blood vessels.
“Measuring an individual’s ability to restore blood circulation after a serious, life-threatening health event, may be useful in choosing treatment options and timing of specialist or GP visits. It may also have implications for susceptibility to other complex diseases, such as cancer.
“We showed testing for a VEGF-A gene variant from a patient’s blood was a useful predictor of how long these patients survived after their heart disease event. This association was most obvious in non-diabetic patients.”
The study reported on 1927 patients from the Coronary Disease Cohort Study that involved patients from Auckland and Christchurch. For approximately 30 percent of these patients, it was not their first episode of serious heart disease.
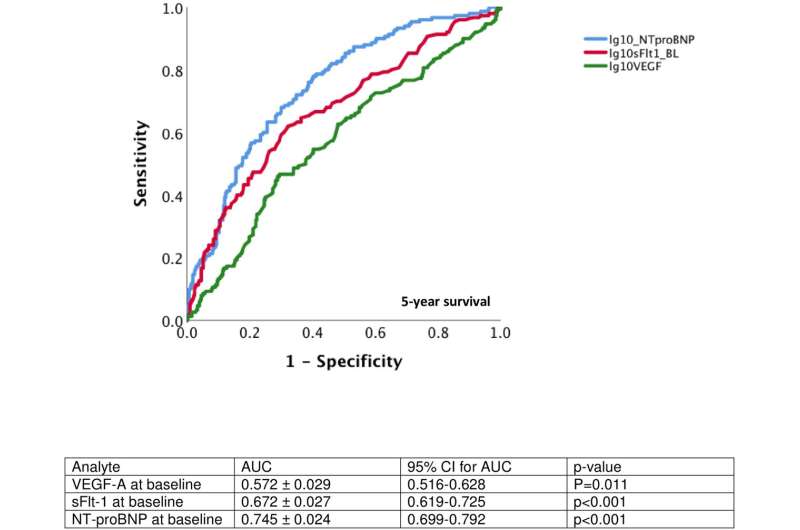
In a subgroup, the researchers also investigated the utility of measuring VEGF-A protein itself from 550 heart patients.
Dr. Palmer says it has been known for some time that VEGF-A plays a role in helping cancer tumors to grow, by helping tumors get a good blood supply.
“In the heart disease field, it’s been suggested that high levels of VEGF-A might be a good thing to help grow new blood vessels around clogging or blocked arteries. The research so far has led to some controversy with some reports showing that more VEGF-A in the bloodstream is associated with better outcome in heart disease.
“While others, including our study, shows high levels of VEGF-A after a heart event is linked to worse outcomes. An explanation for this could be that high VEGF-A levels may signal hearts under stress struggling to restore heart function, but not always rescuing function enough to save badly damaged hearts,” Dr. Palmer adds.
“High levels of VEGF-A in the blood may be being churned out to try and grow new blood vessels in a badly damaged heart, but may not be enough for the patients with the most damaged hearts. About 40 percent more of patients with high VEGF-A are dying within eight years of their original admission to hospital.
Source: Read Full Article