About 38 million people worldwide are living with AIDS. Pharmaceutical treatments can keep the disease in check, but a vaccine remains elusive despite decades of concerted effort. However, a recent discovery at the Duke Human Vaccine Institute (DHVI) brings the goal of an effective vaccine within reach.
One of the ways that HIV, the virus that causes AIDS, outwits the immune system is by dressing like a wolf in sheep’s clothing: It covers itself with sugar molecules, called glycans, just as the body’s own cells do. The disguise isn’t perfect, but it gives the virus a deadly head start on the immune system.
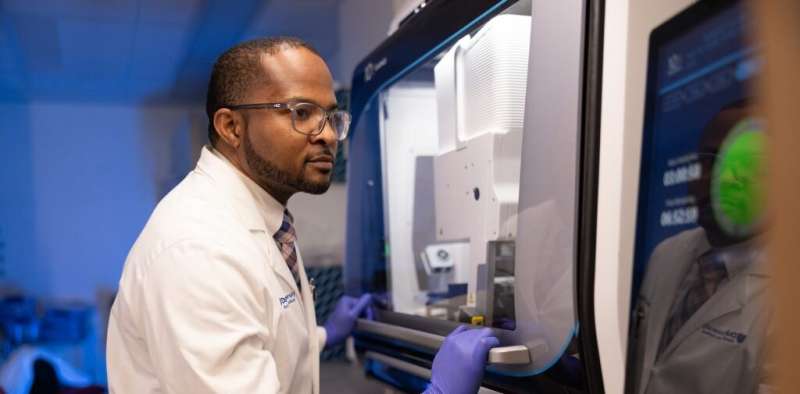
“By the time the immune system realizes the virus is an invader, it’s too late,” says Wilton Williams, Ph.D., director of the DHVI Viral Genetic Analysis Core Facility and associate professor of surgery in the Duke University School of Medicine. “The virus has spread to areas where the immune system can’t get to it.”
The disguise also makes it difficult to create a vaccine since a vaccine’s job is to help the immune system recognize a pathogen. But how can the immune system recognize a virus covered with the same sorts of glycans that also cover human cells?
HIV’s disguise, which scientists call the glycan shield, has one small patch that differs from the glycans on human cells. Scientists have long wanted to target that area with a vaccine. The stumbling block has been the configuration of our antibodies, which are shaped like the letter Y. That shape keeps them from binding effectively to the glycans. It’s as if the key is the wrong shape for the lock.
Scientists working at DHVI, directed by Barton Haynes, M.D., may have recently found a key that will work—a new class of antibodies that are shaped like the letter I instead of Y.
“We’ve found there are antibodies that can target a specific sugar patch on HIV,” Williams says. “We are no longer afraid of the glycan shield.”
The I-shaped antibody isn’t capable of neutralizing HIV right off the bat, but researchers believe it has the potential to evolve into an effective anti-HIV antibody with the encouragement of a series of vaccines.
Williams and the other members of his lab are looking at blood samples from uninfected people to determine the frequency of the I-shaped antibodies. Most, if not all, people likely have them, because they bind to yeast, a ubiquitous pathogen. But the I-shape is much less common than the Y-shape. “We’re looking for a needle in a haystack,” Williams says.
The discovery of the new class of antibodies was very much a team effort at DHVI. “Under one roof, we have a sequencing facility, we have a structural biology facility, we have immunologists doing basic science research,” says Williams. “I collaborate with all those teams. This collaboration helps the science move much faster and puts us in the space of doing innovative work.”
Priyamvada Acharya, Ph.D., who directs the structural biology group at DHVI, says, “Whenever Wilton finds a new antibody, he sends them over to us to visualize them, not only to see whether they are Y- or I-shaped, but to get high-resolution details for where and how they bind and what they interact with.”
Acharya’s lab utilizes the latest equipment for looking at antibodies and HIV proteins, including a Titan Krios cryo-electron microscope, which can take pictures with atomic-level precision. Without this technology, DHVI couldn’t have found the new antibodies.
However, it’s not just the technology that made this discovery possible. “You have to know what you are looking for,” Acharya says. “That’s why people haven’t found these before.” According to Acharya, the I-shaped antibodies are not stable and easily equilibrate to Y-shaped and back, making the I-shape tricky to catch.
The team at DHVI is hard at work to develop a vaccine that can target the new antibodies and lead the immune system, step by step, to an immune response that can prevent HIV infection. “We’re getting close,” Williams says. “It’s a matter of trying to get all the pieces correct to stimulate the immune system and help it respond effectively. We know what we need, but the question is how do we get there.”
Getting there will require intense multidisciplinary collaboration, which has been an integral part of DHVI culture since its founding in 1990. The many advances in immunology and vaccine science that have come out of DHVI since then all rest on that foundation of collaboration among experts in many different disciplines and technologies across the School of Medicine and university.
Source: Read Full Article