New research has uncovered genetic variations that may contribute to the development of non-alcoholic fatty liver disease (NAFLD), the leading cause of liver disease.
NAFLD is major health concern in Western countries, with one in four people, including children, affected.
The international collaboration led by Associate Professor Mohammed Eslam and Professor Jacob George of the Westmead Institute for Medical Research, studied more than 1,000 patients with NAFLD to establish a link between genes and a build-up of fat in the liver, known as hepatic steatosis.
The team found that three genetic variations — FNDC5 rs3480, PNPLA3 1148M, and TM6SF2 E167K — were linked to increased fat in the liver.
Lead author Dr Mayada Metwally said the findings strengthened the link between genetics and liver disease, which could lead to new treatment options.
“Hepatic steatosis is one of the major risk factors for NAFLD, so if we can understand its causes, we can work towards preventing it,” she explained.
“We’ve previously thought that genes such as FNDC5, which help make a protein called irisin, play a role in depositing fat in the liver, but this is the first time we’ve demonstrated the link and identified the mechanisms.
“Our findings show that these genetic variants contribute to liver fat in people with NAFLD. The more variants a person has, the more likely they are to accumulate fat in the liver.”
Left untreated, NAFLD can also cause complications in the heart and kidneys.
“The growing number of people with NAFLD is alarming, particularly since many patients don’t develop symptoms until the condition is advanced,” Dr Metwally said.
“Understanding the genetic causes of NAFLD is crucial. We can now look towards targeting these genetic variations as a potential treatment to slow the progression of disease.”
About the science
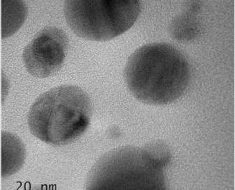
The team discovered how a single-letter variation in the FNDC5 gene mediates differences between those at risk of severe steatosis, and those who are not. The authors show that a particular microRNA is induced in the liver of people with NAFLD.
MicroRNAs are silencers: they stop the ‘messengers’ that transmit information to produce a protein from a gene, in this case, the production of the protective protein FNDC5. The researchers also observed that this ‘bad’ microRNA binds too and represses FNDC5 production.
Source: Read Full Article