Photo: AWS
Over the last almost two years, healthcare has seen organizations rely on technology and the cloud to get accurate, trusted information to patients and direct them to the appropriate resources and care at scale.
From chatbots and remote patient monitoring to telehealth, the industry worked quickly to adapt and find new ways to care for patients. But what does all of this mean for the future of patient care?
Healthcare must look at how access to the right patient data, paired with advanced analytics and machine learning, can enhance medical and scientific insights tied to patient outcomes in an accurate, scalable, secure and timely manner, says Dr. Rowland Illing, director, international public sector health, at Amazon Web Services.
By eliminating barriers and providing greater visibility into a patient’s medical history and then providing bespoke recommendations or materials to support their care, interoperability and tech stand to provide a better patient experience anywhere as well as empower patients to take greater control over their healthcare journey, he said.
Healthcare IT News interviewed Dr. Illing to talk about telehealth, the cloud, machine learning, advanced analytics and much more.
Q. What examples have you seen of telehealth, remote patient monitoring and chatbots in the cloud, and what has been the impact on patients?
A. Telehealth and remote patient monitoring have the potential to revolutionize the delivery of healthcare by improving patient access to care and driving better outcomes, fewer hospital readmissions, greater patient and caregiver satisfaction, and reduced costs.
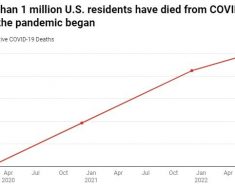
During the COVID-19 pandemic, telehealth and remote monitoring have found their place in routine clinical practice like never before. According to a study published by the Journal of the American Medical Informatics Association, during the pandemic, telehealth services for urgent care have grown by 683% and by 4,345% for non-urgent care.
At Boston-based Beth Israel Deaconess Medical Center (BIDMC), half of telehealth consultations were done by video at the height of the pandemic, with approximately 4,200 patient virtual visits each weekday. As we begin to emerge from the pandemic, BIDMC staff expect telemedicine to continue at the current volume of 20% of all ambulatory care visits.
Remote monitoring has also moved into the mainstream. During the pandemic, a health technology company provided IoT devices to people’s homes that monitored COVID-19 symptoms, along with a platform for data collection. Caregivers were able to track these patients’ vital signs from a centralized dashboard, … identify those who were deteriorating, and provide them with advice or admit them to the hospital.
A paper published in April this year in EClinical Medicine demonstrated that 94% of a cohort of more than 1,700 patients were able to be managed at home (with remote monitoring) who would otherwise have been admitted to hospital.
Of the 6% who deteriorated, they were admitted to hospital with no worse outcomes than would be expected had everyone been admitted. This significantly reduced hospital admissions and increased the number of patients each doctor could manage at a time.
Based on work with a number of organizations, including Halodoc, Doctor Anywhere and Doctor Raskam, we’ve seen telehealth driving better health outcomes in several ways.
1. Access to quality care in underserved communities. Provider shortages, distancing and restrictions, and limited transportation options seriously diminish access to timely and quality care in these areas. When patients are unable to come to a hospital or clinic, telehealth solutions that provide secure, two-way audio, video and text communications provide an effective way to meet patients where they are.
For example, as part of the NYC COVID-19 Rapid Response Coalition, MetroPlus Health helped design, deploy and refine an SMS-based engagement process for high-risk, chronically ill and underserved New Yorkers in need of at-home care and services.
Over a three-week period, the campaign reached up to 10,000 members a day, connecting them to available resources. As a result, thousands of at-risk individuals were connected with necessary services while reducing their exposure to COVID-19.
2. Timely and effective urgent and emergency care. In critical situations, telemedicine can help save lives, reduce the number and cost of emergency room visits, and limit the spread of disease.
For example, telehealth can allow physicians to provide remote care to patients in the moments after a stroke or a heart attack until paramedics arrive. When it’s not clear whether an emergency visit is required, physicians can conduct remote consultations with patients to determine the best course of action.
3. Improved provider productivity. Physicians and frontline staff spend significant time entering detailed data into electronic health record systems and travelling between clinical locations. AI- and machine learning-based telehealth solutions assist medical teams with both diagnosis and clinical notes, and telehealth-based patient visits reduce physician travel.
Telehealth technology, such as virtual nurse assistants and chatbots, facilitate self-service pre-screenings, automate health-information sharing, and assist with diagnostics, freeing up provider time to focus on more patients.
4. Reduced healthcare costs. Telehealth is minimizing the number of routine doctor visits, ER visits, hospitalizations and readmissions through video consultation and remote patient monitoring. For example, the U.S. Veterans Administration estimated an average annual savings of $1 billion with patients who participated in telehealth programs. Other cost savings include reduction of medical transportation and patient travel reimbursement costs.
5. Improved operational efficiency. Healthcare organizations often face operational challenges. In health systems relying on insurance, these include budget and enrollment model forecasting, fraud detection, and waste reduction.
Forecasting services can be used to help predict patient enrollment models and budgets. Using these capabilities, organizations can reduce forecasting from months to hours. They can also proactively identify fraud, waste and abuse within telehealth programs using machine learning models trained to detect financial and transactional anomalies.
Additionally, MedStar Health, the largest not-for-profit healthcare provider for patients in the Maryland and Washington, D.C., region, built a telehealth contact center using Amazon Connect to provide easy communication with doctors and streamline billing for patients. The solution collects metadata about the patient’s visits with their healthcare providers so that bills can be accurately calculated.
6. Continuously improving patient experience. Automatic speech recognition and natural language understanding applications enable providers to offer patients highly engaging, lifelike conversational interactions that recognize the intent of voice and text transactions.
Translation services convert text from one language to another so providers can support patient interactions and medical transcriptions in multiple languages. Personalization services enable provider organizations to send patients timely and relevant communications via email, SMS and other channels. This is particularly effective for communication with patients during a health crisis or during an open enrollment period.
For example, Nye Health in the U.K. has the flexibility to scale its business quickly, easily, and in a secure way to meet the increased demand from clinicians and patients during COVID-19. The service frees up capacity during peak periods, triaging patients so that more urgent cases are prioritized for face-to-face appointments. The platform currently has a reach across more than 10 million patients and is growing by as much as 150% a week, servicing thousands of patient consultations each week.
7. Stronger data security and privacy. Security and privacy are a top priority for organizations and agencies dealing with telehealth, due to federal regulatory and compliance frameworks such as HIPAA, HITRUST and the Federal Risk and Authorization Management Program (FedRAMP). Cloud services today provide a number of capabilities to support data privacy and security, including the ability for customers to encrypt data in transit and at rest.
AWS also offers a Reference Architecture for HIPAA that can help organizations with machine learning workloads that fall within the HIPAA scope. In Europe, AWS supports customers’ compliance to legislation such as the General Data Protection Regulation (GDPR), as well as country-level regulation such as DiGAV in Germany.
Q. You’ve noted that patient data, paired with advanced analytics and machine learning, can enhance medical and scientific insights. Please elaborate.
A. The amount of healthcare data generated globally is increasing exponentially. In particular, we see an increase in data-heavy workloads such as telemedicine, medical imaging, genomics and electronic health records. This will only increase further as remote monitoring devices and wearables become even more common and start adding ‘clinical-grade’ information into patient records.
Healthcare providers running their own data centers are facing an almost overwhelming task of guessing how much storage they will require in the future and how much processing power will be required to run analytics on the data to extract meaningful insights. This is why we are seeing many large providers move into the public cloud to remove these concerns.
An example of this is the U.K. BioBank, the world’s largest and most comprehensive biomedical database, comprising the genomes of 500,000 patients and their associated clinical and biomedical data.
They chose to move to the cloud in order to scale seamlessly and democratize access to both data and analytics. Researchers no longer have to download data onto their own systems and invest in expensive high-performance computing.
They can securely access this data and the most up-to-date machine learning tools on the Research Analysis Platform built by DNAnexus. There are currently 11 petabytes of data on the platform, and this is expected to grow to 40 petabytes by 2025.
Big data, coupled with machine learning, has the power to improve the quality of patient care. According to the Agency for Healthcare Research and Quality (AHRQ), diagnostic errors contribute to about 10% of patient deaths and are the primary reason for medical liability claims.
With the advancements in AI and machine learning, computer vision can aid physicians with medical diagnosis in a number of areas, including radiology, oncology, ophthalmology and dermatology, especially in areas where there may not be experts available to assist patients.
To assist hospitals lacking chest radiologists and to help provide faster diagnoses during the pandemic, the Hospital das Clínicas Innovation Center in Brazil, in partnership with the private sector and federal government, created the RadVid-19 project.
Using this AI platform, any hospital in Brazil can send its chest CTs to the platform, where two AI algorithms interrogate it and return a report with a COVID-19 probability analysis and the extent of the affected lung tissue.
The facility operates 24 hours a day, free of charge to the hospitals using the service, and reports are delivered within 10 minutes.
A great benefit of cloud computing is that machine learning tools are readily available, and can be leveraged by users with a range of different expertise. At AWS, we consider machine learning in three layers. The bottom layer is the framework level for expert practitioners who are comfortable building and managing models themselves.
The middle layer is an integrated development environment called Amazon SageMaker, a fully managed service that removes the heavy lifting, complexity and guesswork from each step of the machine learning process. This allows everyday developers and scientists to successfully use machine learning.
At the top layer, we have managed services that can be incorporated directly into solutions, with no need for building or training by the user. For healthcare, these are services such as Amazon Comprehend and Amazon Transcribe Medical that are able to recognize natural language and automatically extract both structured and unstructured data into machine consumable formats.
These tools, when coupled with the vast amounts of healthcare data being generated, can allow meaningful insights to be extracted from the data at scale.
Q. You mentioned earlier the growth of telemedicine that has taken place during the COVID-19 pandemic. Given the expansion of these services and the ability of patients to seek care anywhere around the world, does this make the issue of interoperability even more pressing?
A. Indeed, the changes have been profound. Over the last 18 months, Brazil has legalized the use of telemedicine, and Australia has made telehealth a part of the national health service going forward.
The Indian government built the eSanjeevani telemedicine platform on AWS in 19 days across four states, free to patients and available 12 hours a day, seven days a week.
This pilot was such a success that it was scaled up to cover all of India, enabling more than one billion people to seek virtual care – 80% of the Indian population. It now provides more than 6,000 consultations a day across 23 states, involving 4,000 doctors in 150 outpatient clinics.
In the U.S., the federal government enabled Medicare to reimburse telemedicine services more comprehensively, while individual states have implemented legislation to improve access to virtual care. In Japan, Canada and many EU countries, frameworks for telehealth provision were already in place, but the pandemic accelerated adoption.
This expansion of telehealth has further highlighted the requirement for interoperability. Gathering patient data in different formats makes meaningful analysis challenging and machine learning laborious. While there is a move to unify the data formats used to collect clinical data, it is not yet comprehensive, despite a mandate in some countries such as the U.S.
Open data standards – for instance, the Fast Healthcare Interoperability Resources (FHIR) and common application programming interfaces for interoperability – are a great way forward, but when a health system uses interfaces that are either proprietary or that conform to older standards, they can fail to support true interoperability.
This results in data that is digitally available but not accessible to the right providers, creating an incomplete view of a patient’s health history. FHIR addresses this issue, helping remove barriers to fast, easy and secure electronic data exchange across the healthcare industry.
Transformation of healthcare data into FHIR format is a key process to enable interoperability. Solutions such as FHIR Works on AWS enable customers to build interoperability into their platforms, as Black Pear has done. Once in FHIR format, both structured and unstructured data can then be extracted, transformed and loaded into analytics and machine learning solutions using tools such as Amazon HealthLake.
I have no doubt that telehealth is here to stay. It has enabled those in need to access healthcare, and it will mature as countries formalize regulatory frameworks. We have only scratched the surface when it comes to the use of chatbots and remote monitoring.
Given the exponential growth of healthcare data, more payers and providers will rely on cloud to scale data storage, analytics and machine learning, leveraging machine learning tools at the appropriate level of the stack. Interoperability will remain a key focus, and with wider adoption of open standards such as FHIR, the ability to extract meaningful insights from patient data will only increase.
Twitter: @SiwickiHealthIT
Email the writer: [email protected]
Healthcare IT News is a HIMSS Media publication.
Source: Read Full Article