Thought LeadersDr. Cicely Fadel and Amir Bein R.D., Ph.D.ResearchersWyss Institute for Biologically Inspired Engineering at Harvard University
Thought LeadersDr. Cicely Fadel and Amir Bein R.D., Ph.D.ResearchersWyss Institute for Biologically Inspired Engineering at Harvard UniversityIn this interview, News-Medical speaks to Dr. Cicely Fadel and Amir Bein Ph.D about their latest research which involved the development of an Environmental Enteric Dysfunction (EED) Chip that reveals the effects of nutrition and genetics on disease in children.
Please can you introduce yourself, tell us about your scientific background, and what inspired your latest research?
Cicely W. Fadel: As an MD/PhD, my passion for using emerging technologies to better understand and more effectively treat human disease has been the driving force behind my many career stages, from bench to bedside. Practicing medicine affords me the privilege of providing care to critically ill newborns and their families. It also highlights the limitations of current therapies and pushes me to pursue a better understanding of disease pathophysiology with the hopes of expanding treatment options. I began this research after gaining a clinical appreciation for how prematurity leads to gut vulnerability in the neonatology world and wanting to gain insight into how malnutrition leads to gut vulnerability in the context of global health.
Amir Bein: As a clinical nutritionist and cell biologist (Ph.D., RD), my research has focused for over a decade on modeling intestinal diseases in vitro and studying the effects of nutritional conditions on the health and functionality of the intestine. One of my main research interests is interdisciplinary work combining engineering and biophysics to enhance cell biology research capabilities. This experience and background led me to the field of Organs-on-Chips, which provides unprecedented capabilities in studying human organ-level responses to different conditions and aspects of disease pathways. This background in nutrition, cell biology, intestinal disease modeling, and the organ chip tool made it possible to take this work creating an organ chip EED model and get more insight into the effect nutrition has on this disease.
For those unfamiliar, could you introduce environmental enteric dysfunction, its causes, symptoms, and the currently available treatments?
Environmental enteric dysfunction is a form of intestinal vulnerability that occurs when a combination of malnutrition and constant exposure to pathogens leads to chronic inflammation of the gut. This manifests as thinning of the intestinal lining, growth of abnormal gut bacteria, weakening of the intestinal barrier, and failure to absorb nutrients properly. The long-term consequences include poor response to oral vaccines, predisposition to infection, physical and cognitive stunting, and death. Early efforts at treatment focused on nutrient replacement, but these approaches have only had limited success.
Image Credit: Marko Aliaksandr/Shutterstock.com
In your study, you utilized an Organ-on-a-chip technology. What advantages does this micro physiological system provide when studying disease?
The content of cells is important, but so is the context of where cells live. The environment surrounding a cell provides it with chemical and mechanical cues that influence its behavior. When a cell is grown in a static two-dimensional culture dish, it is missing these important cues. With Organ-on-a-chip technology, you can provide these crucial cues, and when you look at the genes being expressed by the cells, they more closely resemble those expressed by cells living inside organs in the human body.
Studying a multifactorial disease, such as EED, raises substantial methodical and modeling challenges. At present, there are only a few murine models and no existing human in vitro models that can be used to study this disease. Our Organ-on-a-chip model of EED can be leveraged to elucidate disease pathophysiology and may enable the development of new prevention and therapeutic measures.
How was your specific chip developed, and then how did you replicate EED in these chips?
This chip was developed in close collaboration with researchers at Agha Khan University in Pakistan. They were able to culture organoids using intestinal samples from EED clinical trial patients. These organoids were used to generate the living intestinal epithelium on the EED chips. We then exposed the chips to cell culture media lacking key nutritional components also implicated in clinical EED.
When studying the gene expression patterns of the cells in their EED Chips vs. Healthy Chips, what were your main findings?
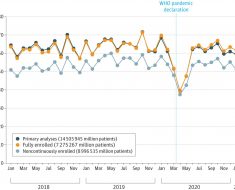
When EED patient-derived chips are exposed to nutritional deficiency, they exhibit transcriptional changes similar to those seen in clinical EED biopsy specimens from patients in Pakistan, Bangladesh, and Zambia. When specifically compared to the data from Pakistani EED patients, six out of the top ten genes that are upregulated in clinical biopsy specimens were also upregulated in our nutritionally deficient EED Chips.
Image Credit: arleksey/Shutterstock.com
Affected pathways included upregulation of genes related to antimicrobial defense, chemokine production, and amino acid starvation, with downregulation of genes related to fatty acid uptake and utilization, brush border structural integrity, metallothionein production, metabolism and digestion, and cellular mitosis.
Within the content of EED, what did your study tell us about nature vs. nurture?
A key advantage of Organ-on-a-chip technology we could leverage in this study is its modularity. By adding EED patient intestinal epithelium and nutritional deficiency independently, we discovered that transcriptionally, EED intestinal epithelium responds differently when challenged with nutritional deficiency. This suggests that both nature and nurture play a role in disease pathophysiology. While this may seem surprising for an endemic disease whose diagnosis is based on gut morphology, it is important to note that this work focused on an important clinical subpopulation of EED patients who are recalcitrant to nutritional intervention. Their severe disease may be uniquely driven by a stress response triggered by the contest of predisposing genetic or epigenetic factors.
How do you foresee disease-on-a-chip technologies furthering the understanding of the cause of diseases?
One of the main hurdles in disease modeling is mimicking human organ-level responses within a simplified in vitro system. Organs-on-a-chip technology provides this capability by allowing compartmentalization and control over mechanical cues that generate physiologically relevant functionality of the miniaturized organs. With this, disease modeling on a chip provides more accurate results when studying disease mechanisms and responses to different perturbations/treatments. By using this approach, we can now get better insight into the core and combined causes of a disease and the potential efficacy of treatments.
What is next for yourself and your research?
Cicely Fadel: In addition to continuing my clinical work, I will utilize my clinical and research background as a Senior Program Officer at the Bill and Melinda Gates Foundation for the Maternal, Newborn, and Child Health Discovery & Tools team. This position within the Gender Equality Division will focus on developing a portfolio of emerging technologies and products to advance neonatal health care globally. This work will harness my expertise in Neonatology and experience in cutting-edge, innovative investigational approaches to address major disease causes in low- and middle-income countries.
Amir Bein: With my experience in cell biology and micro physiological systems, my research focuses on utilizing Organ-on-a-chip to study specific organ and multi-organ responses. In my current work, leading the biology research and development of a Bio-Ai platform at Quris Technologies, I am focusing on the intersection of organs on chips models with real-time biosensing, high throughput screening, and strong Ai to predict drug toxicity in clinical studies.
About Cicely Fadel
Dr. Cicely Fadel cares for critically ill newborns at Beth Israel Deaconess Medical Center while working at the Bill and Melinda Gates Foundation to promote global gender equality through maternal and newborn health. Cicely is currently an Attending Neonatologist and Instructor in Pediatrics at Harvard Medical School and a Senior Program Officer on the Maternal, Newborn, and Child Health Discovery and Tools team at the Gates Foundation. She obtained her M.D. and a Ph.D. in Neuroscience from Yale University before completing her pediatric residency and serving as a chief resident at Children’s National Medical Center in Washington, DC. She completed her neonatology fellowship at the Harvard Neonatal-Perinatal Fellowship Program, where she was a chief fellow. Prior to joining the Gates Foundation, Cicely utilized cutting-edge Organ Chip technology at the Wyss Institute for Biologically Inspired Engineering to study pediatric intestinal vulnerability in the context of prematurity and malnutrition.
Cicely is currently an Attending Neonatologist and Instructor in Pediatrics at Harvard Medical School and a Senior Program Officer on the Maternal, Newborn, and Child Health Discovery and Tools team at the Gates Foundation. She obtained her M.D. and a Ph.D. in Neuroscience from Yale University before completing her pediatric residency and serving as a chief resident at Children’s National Medical Center in Washington, DC. She completed her neonatology fellowship at the Harvard Neonatal-Perinatal Fellowship Program, where she was a chief fellow. Prior to joining the Gates Foundation, Cicely utilized cutting-edge Organ Chip technology at the Wyss Institute for Biologically Inspired Engineering to study pediatric intestinal vulnerability in the context of prematurity and malnutrition.
About Amir Bein
Amir Bein (PhD, RD), is VP of Biology at Quris Technologies – a Bio-Ai company developing a platform for the prediction of drug toxicity before progressing to clinical studies. Amir earned a Ph.D. from the Hebrew University of Jerusalem, where he graduated as a laureate of The Harry and Sylvia Hoffman Leadership and Responsibility Program for outstanding Ph.D. students. He has extensive research experience in in-vitro disease and organ modeling, combining cell biology and micro physiological systems.
Before joining Quris, he led cutting-edge high-risk research at Wyss Institute for Biologically Inspired Engineering at Harvard University, developing and utilizing Organ Chip technology to study disease mechanisms, model inf ectious conditions such as Corona Virus, and test repurposing of drugs.
ectious conditions such as Corona Virus, and test repurposing of drugs.
Posted in: Thought Leaders
Tags: Amino Acid, Bacteria, Biopsy, Cell, Cell Biology, Cell Culture, Chemokine, Child Health, Children, CHIP, Chronic, Clinical Trial, Digestion, Disease Modeling, Drugs, Efficacy, Gene, Gene Expression, Genes, Genetic, Global Health, Health Care, High Throughput, in vitro, Inflammation, Intestinal Disease, Malnutrition, Medical School, Medicine, Metabolism, micro, Mitosis, Morphology, Neonatology, Neuroscience, Newborn, Nutrients, Nutrition, Organoids, Pathophysiology, Pediatrics, pH, Research, Stress, Virus

Written by
Danielle Ellis
Danielle graduated with a 2:1 in Biological Sciences with Professional Training Year from Cardiff University. During her Professional Training Year, Danielle worked with registered charity the Frozen Ark Project, creating and promoting various forms of content within their brand guidelines.Danielle has a great appreciation and passion for science communication and enjoys reading non-fiction and fiction in her spare time. Her other interests include doing yoga, collecting vinyl, and visiting museums.
Source: Read Full Article