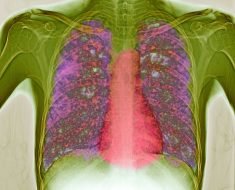
The oral sphingosine-1-phosphate receptor modulator ozanimod is significantly more effective than placebo for treating patients with moderate to severe ulcerative colitis, regardless of prior biologic exposure, based on results of the phase 3 True North trial.
Although improvements were seen across all patients, those who had previously used biologics took slightly longer to respond to treatment, which suggests that any initial improvements with ozanimod warrant continuation of therapy to achieve full effect, reported to lead author Bruce E. Sands, MD, of Icahn School of Medicine at Mount Sinai, New York, and colleagues.
“[Ulcerative colitis] patients previously treated with a biologic agent may be less likely to respond to another advanced treatment,” Sands said during a presentation at the annual meeting of the American College of Gastroenterology.
Sands and colleagues evaluated this possibility in the True North trial, which previously demonstrated superior efficacy and safety of ozanimod over placebo through 1 year.
The present dataset included a double-blinded cohort of 639 patients (cohort 1), among whom 213 took placebo and 426 took ozanimod, and an open-label cohort of 353 patients who took ozanimod (cohort 2). Outcomes included clinical remission, clinical response, endoscopic improvement, and mucosal healing.
During induction (through week 10), biologic-naive patients in both cohorts generally responded better to ozanimod than those who had received at least one prior biologic. Patients who had received two or more biologics showed less improvement than those who had received only one prior biologic.
For example, in cohort 1, 53% of biologic-naive patients in the ozanimod group achieved a clinical response, compared with 50% of patients who had received one prior biologic, and just 27.2% of patients who had received two or more biologics.
With maintenance therapy, however, these differences faded. Among participants continuing ozanimod through week 52, 60.7% of biologic-naive patients achieved a clinical response, compared with 60.5% of those who had taken one prior biologic, and 55.3% of patients who had taken two or more prior biologics.
“Ozanimod treatment for up to 52 weeks in patients with moderate to severe ulcerative colitis improved clinical symptoms, mucosal ulcerations, and reduced cellular inflammation in both biologic-exposed and biologic-naive patients,” Sands concluded. “Greater efficacy was observed in biologic-naive patients, followed by patients with prior exposure to one biologic, at induction; however, all groups had benefits at end of maintenance. Patients with prior biologic use may require additional time to respond to treatment.”
Bradley Morganstern, MD, codirector of the IBD Center at Stony Brook (N.Y.) Medicine, called the study “a really important analysis” that addresses a common clinical decision.
“We often see a lower response rate among patients previously on biologics, but we have very limited data to guide us on how to choose a second-line agent,” Morganstern said during an interview.
He said the current findings encourage use of ozanimod for patients who didn’t respond to other biologics.
“The takeaway is that just because someone didn’t respond to a biologic in the past doesn’t mean they won’t respond to this,” Morganstern said. “They actually have a very good chance of responding – similar to the rest of the population that was never on medication.”
He went on to explain that exact treatment sequencing remains unclear, although ozanimod is a strong candidate in the second line.
“We can’t 100% say where it [ozanimod] fits in,” Morganstern said, “but we should certainly place it high up in the algorithm for patients who have failed a biologic. This should strongly be considered as a second-line agent.”
Morganstern said that he looks forward to long-term findings from True North beyond 1 year, “in terms of maintaining response,” and additional safety data.
The study was funded supported by Bristol-Myers Squibb. The investigators disclosed additional affiliations with AstraZeneca, AbbVie, Amgen, and others. Morganstern has previously spoken for Bristol-Myers Squibb.
This article originally appeared on MDedge.com, part of the Medscape Professional Network.
Source: Read Full Article