Pelvic exams are an indispensable part of gynecological care and are used to screen for conditions, such as cervical cancer, that affect millions of patients every year. Unfortunately, pelvic exams can be challenging for both physicians and patients. Since the beginning of this field, gynecologists have struggled with the inward collapse of lateral vaginal walls during a pelvic exam, making it difficult to carry out a proper analysis.
“Any obstetrician gynecologist, or OB/GYN, knows that this is a problem with pelvic exams, and it is usually associated with higher body mass index,” said Peggy Palsgaard, a fourth-year medical student at the Carle Illinois College of Medicine.
Routine pelvic exams are carried out using a speculum, which has a handle and two blades. The upper and lower blades pull back the front and back vaginal walls, respectively. However, there is no mechanism to pull back the lateral walls, which causes them to bulge inward. Unfortunately, this complication can cause more patient discomfort during the exam and can lead to misdiagnosis.
Dr. Rahul Yerrabelli, a former medical student at the Carle Illinois College of Medicine and a first-year OB/GYN resident at Reading Hospital, Pennsylvania; Dr. Ashkhan Hojati, a former medical student at the Carle Illinois College of Medicine and a first-year anesthesiology resident at John H. Stroger, Jr. Hospital, Illinois; and Palsgaard noticed this problem during their medical training and wanted to find an effective solution.
“Although people have focused on designing better speculums, they haven’t been widely adopted. We wanted to focus on a traditional speculum and focus on a solution that can be used easily,” Palsgaard said.
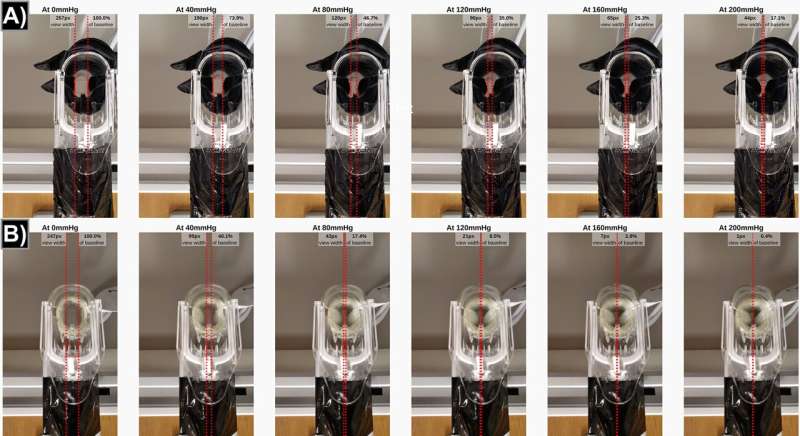
Currently, physicians repurpose gloves or condoms to act as a covering around the speculum. Even so, no peer-reviewed articles have compared these two approaches. The researchers used a blood-pressure cuff to test how much pressure a speculum could withstand before collapsing. They covered it with either a glove or a condom and collected images to see which sheath was more effective in preventing collapse.
“We were surprised to find that in our experiment, condoms were not useful, which doesn’t mean that they can’t be useful in clinics. However, nitrile gloves were the best; they could prevent collapse without restricting the speculum movement,” Palsgaard said.
“These gloves are always present in the exam room and are a part of everyday practice—so this simple solution is accessible in any clinical setting,” said Amy Wagoner Johnson (EIRH/RBTE), a professor of mechanical science and engineering and professor and Head of the Department of Biomedical and Translational Science at the Carle Illinois College of Medicine.
Although the study did not involve patients, the authors are interested in seeing whether it can improve the patient experience. “Our work does not account for how experienced a physician is or how comfortable a patient is if you have to redo the exam with or without a glove,” Palsgaard said. “Ideally, you would try the different methods, but it would be difficult because you’re subjecting a patient to multiple pelvic exams.”
The paper is published in the journal PLOS ONE.
More information:
Rahul Sai Yerrabelli et al, Improving visualization of the cervix during pelvic exams: A simulation using a physical model of the speculum and human vagina as a steppingstone to reducing disparities in gynecological cancers, PLOS ONE (2023). DOI: 10.1371/journal.pone.0283145
Journal information:
PLoS ONE
Source: Read Full Article