SARS-CoV-2 spike protein's role in lung injury unraveled: promising new approach uncovered
In a recent study published in Scientific Reports, researchers investigated the effect of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spike (S) protein subunit 1 (S1) on the pulmonary endothelium.
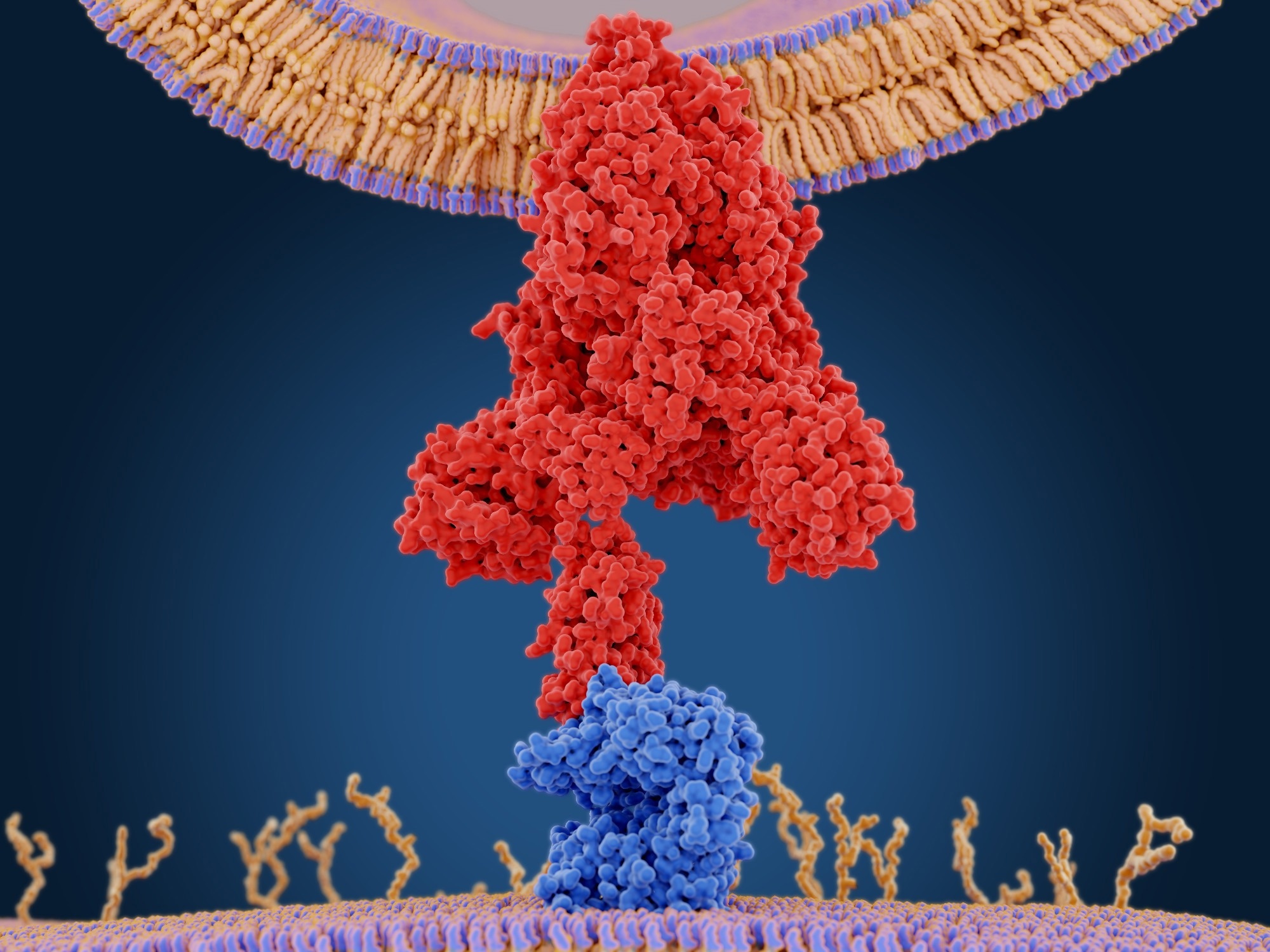 Study: SARS-CoV-2 spike protein induces lung endothelial cell dysfunction and thrombo-inflammation depending on the C3a/C3a receptor signalling. Image Credit: JuanGaertner/Shutterstock.com
Study: SARS-CoV-2 spike protein induces lung endothelial cell dysfunction and thrombo-inflammation depending on the C3a/C3a receptor signalling. Image Credit: JuanGaertner/Shutterstock.com
Background
The coronavirus disease 2019 (COVID-19) caused unprecedented morbidity and mortality across the globe. Studies have reported that the SARS-CoV-2 S1 protein interacts with endothelial cells.
However, data on the detrimental effects of the protein on the pulmonary vasculature and mechanisms underlying SARS-CoV-2 infections are limited.
About the study
In the present in vivo study, researchers assessed SARS-CoV-2 S1-induced endothelial cell damage in COVID-19 pathogenesis.
To increase SARS-CoV-2 S1 binding activity, the researchers employed transgenic murine animals with endogenous murine angiotensin-converting enzyme 2 (ACE2) protein sequences substituted by human ACE2 complementary deoxyribonucleic acid (cDNA). The murine mice were administered intravenously with 35.0 grams (g) of the SARS-CoV-2 S1 protein and killed after three and seven days.
C3 deposits in the pulmonary tissues were assessed to study the deleterious function of complement activation in the onset of pulmonary vascular damage in hACE2-expressing mice infused with S1. The total number of von Willebrand factor (vWF)-labeled lung arteries positive for C3 was assessed to determine the quantity of C3 deposits in the pulmonary vasculature.
The researchers additionally examined the expression of cluster of differentiation 46 (CD46), an outer complement modulator reported to suppress C3 convertase production via the alternative, traditional, and lectin routes.
They also investigated the potential activities of the C3a/C3a receptor (C3aR) axis in SARS-CoV-2 S1-induced damage to pulmonary tissue by examining the levels of certain C3aR at various time points across several pulmonary compartments.
To determine if S1 infusion caused pulmonary vascular cell injury in hACE2-expressing mice, the team quantified the number of biomarkers associated with thrombo-inflammatory processes, such as thrombomodulin (TM). Transmission electron microscopy (TEM) was used to examine the pulmonary tissues of hACE2-expressing animals a week after the S1 injection.
The researchers evaluated the effects of daily injection of a C3a receptor antagonist (C3aRa), SB290157, beginning eight hours after the SARS-CoV-2 S1 infusion in hACE2-expressing animals to establish that complement activation is critical in potentiating the S1-induced endothelial damage in the pulmonary tissues.
They also investigated the effect of C3aRa on inflammatory cell infiltration in the lungs of the S1-treated murine animals. Immunofluorescence analysis was performed, and particular MAC2 and GR1 levels were evaluated to quantify macrophages and neutrophils, respectively.
Results
In mice transgenic for human ACE2, S1 injection induced early loss of lung endothelial thromboresistance at three days, resulting in thrombomodulin loss and increased vWF levels.
S1 exocytosis and endothelial activation were sustained, with a considerable increase in fibrin(ogen) deposits co-stained with CD41-positive thrombocytes in the vasculature as a response to SARS-CoV-2 S1. C3aRa treatment inhibited C3a/C3aR activation and pulmonary C3 deposition, reducing vascular thrombi inflammation and fibrosis.
Histopathological evaluation of the pulmonary tissues at seven days showed diffuse alveolar damage, thickening of the alveolar septa, and hypercellularity in the pulmonary tissues.
A significant reduction in CD46 protein expression in alveolar epithelial and endothelial cells was observed. TEM analysis showed swelling of the endothelium in certain regions of the pulmonary circulation and arterioles.
SB290157 treatment significantly reduced SARS-CoV-2 S1-induced endothelial C3 deposition at seven days, with CD46 restoration. C3aRa treatment also restored TM expression and reduced von Willebrand factor staining in the vascular wall within seven days.
In the pulmonary tissues a week after the SARS-CoV-2 S1 infusion, significant deposition of GR1-positive neutrophils and MAC2-positive macrophages was observed, indicative of early complement activation was crucial in the recruitment of inflammatory cells into the pulmonary tissues. C3aRa treatment was effective in preventing SARS-CoV-2 S1-induced formation of NETs.
C3aRa treatment preserved the alveolar structure of the SARS-CoV-2 S1-infused hACE2-expressing murine animals at seven days, reducing morphological damage to the alveoli and fibrosis in the pulmonary parenchyma.
The observation of a C3aR antagonist blocking endothelial C3 deposition can be explained by previous research that showed that C3a promotes the exocytosis of Weibel-Palade bodies, resulting in vascular surface recruitment that releases prothrombotic P-selectin, tissue plasminogen activator (tPA), and vWF.
Conclusions
The study findings showed that SARS-CoV-2 S1 stimulates vascular dysfunction and complement activation, which is crucial for pulmonary thrombi-inflammatory damage. The lung injury is characterized by early endothelial dysfunction, leading to thrombo-inflammatory and fibrotic damage.
The lung injury is prominent three days after injection and is characterized by TM loss and increased vascular vWF.
Early complement activation coincided with endothelial cellular dysfunction, with C3 deposition in both epithelial and endothelial cells and elevated C3aR expression.
The findings suggest that C3a and C3aR are potential therapeutic targets for COVID-19 patients, with early treatment with complement inhibiting agents being preferred for severe cases.
-
Perico, L. et al. (2023) "SARS-CoV-2 spike protein induces lung endothelial cell dysfunction and thrombo-inflammation depending on the C3a/C3a receptor signalling", Scientific Reports, 13(1). doi: 10.1038/s41598-023-38382-5. https://www.nature.com/articles/s41598-023-38382-5
Posted in: Medical Science News | Medical Research News | Medical Condition News | Disease/Infection News
Tags: ACE2, Angiotensin, Angiotensin-Converting Enzyme 2, Cell, Coronavirus, covid-19, Electron, Electron Microscopy, Endothelial cell, Enzyme, Fibrosis, in vivo, Inflammation, Lungs, Microscopy, Mortality, Neutrophils, Protein, Protein Expression, Receptor, Research, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Syndrome, Transgenic, Vascular, Vasculature

Written by
Pooja Toshniwal Paharia
Dr. based clinical-radiological diagnosis and management of oral lesions and conditions and associated maxillofacial disorders.