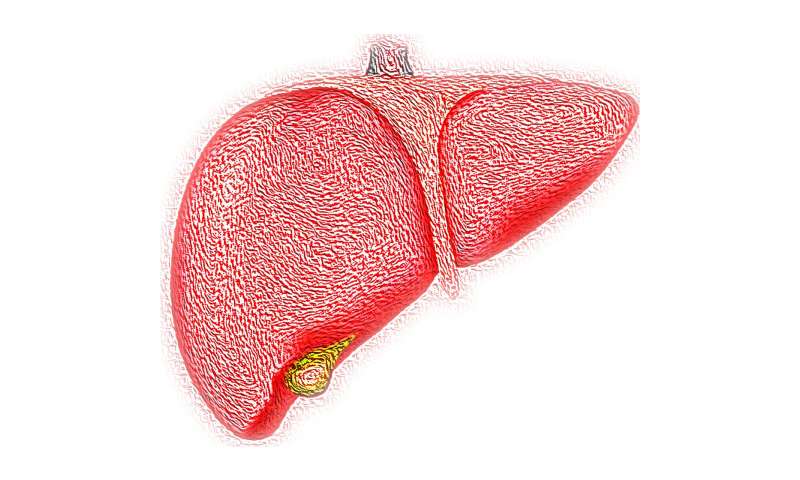
In a world first, scientists have created the human developmental liver cell atlas that provides crucial insights into how the blood and immune systems develop in the foetus. It maps changes in the cellular landscape of the developing liver between the first and second trimesters of pregnancy, including how stem cells from the liver seed other tissues to support the high demand for oxygen needed for growth.
The atlas, published today in Nature, was created by researchers from the Wellcome Sanger Institute, Wellcome—MRC Cambridge Stem Cell Institute, Newcastle University, University of Cambridge and their collaborators. It is a comprehensive, high-resolution resource that improves our understanding of normal development and assists medical efforts to tackle diseases, such as leukaemia and immune disorders, which can form during development.
Until now, it was unknown precisely how the blood and immune systems develop in humans—a process known as haematopoiesis. As adults, it is bone marrow that creates our blood and immune cells. But in early embryonic life, the yolk sac and liver play a major role in making blood and immune cells. These cells subsequently seed peripheral tissues such as skin, kidney and finally bone marrow.
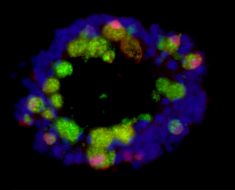
Scientists used single cell technology to analyse 140,000 liver cells and 74,000 skin, kidney and yolk sac cells. By isolating cells from the developing liver, they could identify them by what genes they were expressing and see what the cells looked like. Haematopoietic cells in sections of developmental liver were ‘tagged’ using heavy metal markers so researchers could map each cell to its location.
Professor Muzlifah Haniffa, a senior author of the study from Newcastle University and Senior Clinical Fellow at the Wellcome Sanger Institute, said: “Until now research in this area has been a little bit like blindfolded people studying an elephant, with each describing just a small part of it. This is the first time that anyone has described the whole picture, how the blood and immune systems develop in such detail. It’s been an extraordinary, multidisciplinary effort that is now available as a tool for the whole scientific community.”
A developing foetus requires huge amounts of oxygen to fuel growth. The research discovered that during development, ‘mother’ haematopoietic stem cells stay in the liver. But as the liver alone cannot supply sufficient red blood cells, the next generation ‘daughter’ cells—known as progenitor cells—travel to other tissues. They mature in places such as the skin, where they develop into red blood cells to help meet the high demand for oxygen.
Dr. Elisa Laurenti, a senior author from the Wellcome—MRC Cambridge Stem Cell Institute and the Department of Haematology at the University of Cambridge, said: “We knew that as adults age our immune system changes. This study shows how the liver’s ability to make blood and immune cells changes in a very short space of time, even between seven and 17 weeks post-conception. If we can understand what makes the stem cells in the liver so good at making red blood cells, it will have important implications for regenerative medicine.”
Researchers also mapped genes known to be involved in immune deficiencies to see which cells were expressing them. Gene mutations can lead to immune disorders such as leukaemia, and it is hoped that by understanding how the healthy developing liver functions, it will be possible to understand how immune disorders arise and even how to treat them.
Dr. Sarah Teichmann, a senior author from the Wellcome Sanger Institute, University of Cambridge and co-chair of the Human Cell Atlas Organising Committee, said: “The first comprehensive cellular map of the developmental liver is another milestone for the Human Cell Atlas initiative. The data is now freely available for anyone to use and will be a great resource to better understand healthy cellular development and disease-causing genetic mutations.”
Source: Read Full Article