A new Tel Aviv University study addresses the challenges of nanoparticle-based cancer-targeting strategies. It also suggests ways of refocusing the collaborative work of cancer researchers and clinicians to move the field forward from “the bench” to the patients.
The study follows landmark research published 10 years ago in Nature Nanotechnology that reviewed the full potential of actively targeted nanocarriers to revolutionize cancer care. The opinion piece garnered over 5,000 citations, making it one of the most influential analyses on the subject to date. That study was written by Prof. Dan Peer, director of the SPARK Tel Aviv Center for Translational Medicine at TAU’s Faculty of Life Sciences, and Jeffrey Karp, principal investigator at Brigham and Women’s Hospital and a professor at Harvard Medical School, Harvard University.
The updated review by Prof. Peer, Prof. Karp, Daniel Rosenblum, a doctoral student in Prof. Peer’s lab, and Dr. Nitin Joshi, an instructor at Harvard Medical School, was published recently in Nature Communications.
A hard road from the lab to the clinic
“When Dan and Jeff’s paper was published 10 years ago, there was great hope that nanocarriers in general and actively targeted nanocarriers in particular would transform cancer therapy,” Rosenblum says. “We’ve made significant progress towards understanding the interaction of nanocarriers with tumor cells and tissues since then, but the clinical translation has been limited.”
“Few nanocarriers have been approved for clinical use, and none of the actively targeted nanocarriers have advanced past clinical trials,” Dr. Joshi adds. In the new paper, the authors discuss several reasons for this, including a lack of preclinical models that accurately mimic human tumors. They also emphasize the need not only for patient evaluation before treatment with nanocarriers, but also for clinical trial pathways appropriate for this new generation of drugs.
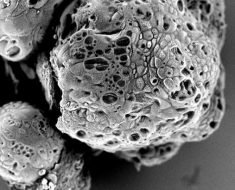
“We detailed what existed in the arsenal at that time, the challenges that lay ahead and how we wanted the future of specific tumor-targeting to look,” says Prof. Peer. “We explored all the available nanoparticle options with which to penetrate tumors. We were sure the future was bright.
“But in the past 10 years, the Food and Drug Administration (FDA) has approved only 15 passively targeted nanocarriers. There have been some 40,000 studies published about active cellular targeting, but none of the approaches have advanced past clinical trials. What’s wrong with this picture?”
It’s complicated
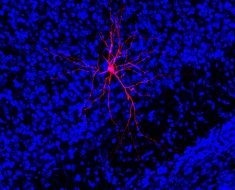
According to the new review, what’s wrong is that cancers have flummoxed researchers by being even more complex in nature than previously believed. “They change and evolve all the time, are heterogeneous in composition and eventually gain resistance,” Rosenblum says. “We need to be able to target many kinds of cancer cell types, and we need the systems to be as simple as possible. But they have to be versatile too. We emphasize the idea of developing personalized nanocarriers based on the type of cancer and its biomarker profile.”
The authors suggest that to move the field forward, the FDA and European Medicines Agency (EMA) must change their regulatory processes. “We have to adopt the regulation process to the new type of drugs,” Dr. Joshi says.
“We need to conduct trials on humans—trials that provide more insights into the interaction of nanocarriers with human biology,” Prof. Karp says. “We can then use these to drive the development of next-generation nano-targeted platforms.”
Rosenblum says the key to future success also lies in developing animal models that better resemble human tumors and preselecting patients with a high likelihood of responding to nanocarrier-based cancer treatments.
The authors argue that technological solutions such as focused ultrasound and companion diagnostics, coupled with biological solutions such as overcoming the cellular barriers and increasing particle payloads at the target site, will also increase the likelihood of successful treatment.
Source: Read Full Article