Melanoma is the least common but one of the most deadly skin cancers. It accounts for only about one percent of all cases globally, but the majority of skin cancer deaths. Accurate, timely and reliable diagnosis of cutaneous melanoma remains a significant challenge in dermatopathology. Investigators report in the Journal of Investigative Dermatology, published by Elsevier, on a novel strategy for using microRNA (miRNA) biomarkers to detect melanoma cells in skin tumors even when the tumor contains predominantly benign cells.
“Although cutaneous melanoma is curable when detected early, the process of differentiating between malignant lesions and the more prevalent benign lesions, such as melanocytic nevi, is challenging,” explained lead investigator Robert L. Judson-Torres, Ph.D., formerly at the University of California, San Francisco (UCSF) and currently with Huntsman Cancer Institute and Department of Dermatology at the University of Utah, Salt Lake City, UT, USA. “Discordance rates across dermatopathologists and care centers are high. Consequently, whether a patient is accurately diagnosed early can depend on where the patient lives.”
Molecular biomarkers such as miRNAs are potentially valuable candidate biomarkers for many conditions and diseases including the diagnosis of melanoma. However, while hundreds of miRNAs have been identified as differentially expressed in melanomas compared to benign melanocytic lesions, there has been limited consensus across studies, limiting their effective use.
According to Dr. Judson-Torres and co-investigators one of the strengths of a molecular approach to melanoma diagnosis is the potential for a truly objective test—where an accurate diagnostic score can be generated and reproduced, regardless of who performs the assay. However, gene expression-based molecular approaches are easily confounded by tumor and tissue heterogeneity. They report a new strategy for overcoming this barrier.
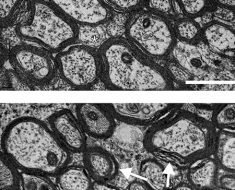
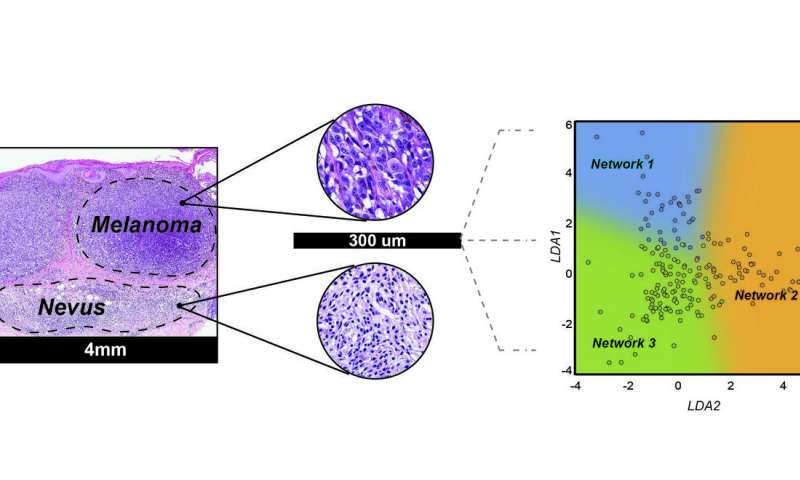
In this study, investigators used machine learning to identify miRNAs, molecules that permit the consistent diagnosis of malignant melanoma from benign moles. They first identified tumor heterogeneity and patient age as the variables that most frequently confuse miRNA-based melanoma diagnostics. Again, using a machine-learning approach, they identified miRNA expression ratios that were both predictive of diagnosis and uninfluenced by these variables. They evaluated 82 biopsied melanocytic lesions with known outcomes (41 neoplasms diagnosed as nevi and 41 diagnosed as melanoma) from the archives of the University of California at San Francisco Dermatopathology Section. Using this new method, lesions were classified with 81 percent sensitivity and 88 percent specificity and results were uninfluenced by tumor content of the sample or patient age.
“We found that by developing a classifier based on a ratio of diagnostically important miRNA we could provide a more robust biomarker that was less susceptible to changes in tumor cell content and platform allowing for a test that could be used on a greater variety of patient samples,” said Rodrigo Torres, Ph.D., lead author on the study.
Numerous studies have analyzed miRNA expression at different stages of melanoma progression, collectively identifying over 500 miRNAs enriched in nevi or melanomas, most of which have not reproduced with external validation sets. Dr. Judson-Torres and colleagues were able to refine this extensive list to six miRNAs that reproducibly distinguish nevi from melanoma across independent datasets and profiling platforms. They were able to further use these findings to identify eight miRNA ratios that are predictive of diagnosis, but unaffected by other confounding variables. Future studies are needed to determine the accuracy of this method in ambiguous cases and to determine whether it can predict metastasis or overall survival.
“MiRNAs are highly stable and measuring them is cheap, easy and requires little tissue. Importantly, this new approach can identify just a few malignant melanoma cells, even when the majority of a tumor is benign. Our hope is that with full clinical validation of our approach, all patients can receive the same level of diagnostic accuracy, regardless of where they live. The early and accurate diagnosis of melanoma is paramount for optimizing patient outcome,” Dr. Judson-Torres added.
“In addition to improving the diagnostic accuracy for melanoma, this technique also has the potential to help catch melanomas earlier, when the tumor is entirely curable, which would significantly impact patient care,” stated Maria L. Wei, MD, Ph.D., a co-investigator on the study, and Director of the UCSF Helen Diller Family Comprehensive Cancer Center Melanoma Surveillance Clinic, San Francisco, CA, USA.
Source: Read Full Article