For at least 20 years, research has shown that for many people, moderate consumption of alcohol can protect the heart, but the reason for this is poorly understood. Now, study conducted at the University of São Paulo’s Biomedical Science Institute (ICB-USP) in Brazil suggests that this cardioprotective mechanism may be associated with activation of ALDH2 (aldehyde dehydrogenase-2), a mitochondrial enzyme that helps rid the organism of both the toxic byproducts of alcohol digestion and a type of reactive molecule produced in heart cells that can suffer major damage, such as that caused by a heart attack.
“Our data suggest moderate exposure to ethanol causes minor stress in heart cells, but not enough to kill them. Intracellular signaling is reorganized as a result, and heart cells eventually create a biochemical memory to protect against stress, also known as preconditioning. When the cells are submitted to a higher level of stress, they know how to deal with it,” said Julio Cesar Batista Ferreira, a professor in ICB-USP’s Anatomy Department and principal investigator for the research project. The results have been published in Cardiovascular Research.
To study the cardioprotective effects of alcohol at the cellular level, the researchers simulated a condition similar to myocardial infarction in mouse hearts kept alive in an artificial system. In this ex vivo model, the heart continues to beat outside the body for several hours while being perfused with an oxygenated and nutrient-enriched solution.
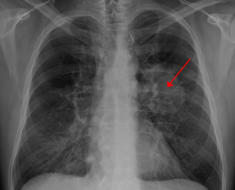
The scientists then simulated a clinical condition known as ischemia-reperfusion injury by interrupting the flow of oxygen and nutrients to the heart for 30 minutes. When the flow was restarted, the heart began beating again slowly, and after an hour, the researchers assessed the damage. In this model, approximately 50 percent of cardiac cells die on average unless there is some type of intervention.
“Lack of oxygen used to be considered the main cause of damage, but research has shown that during ischemia, the cells change their metabolism and enter a sort of dormant state. When the artery is unblocked [reperfusion], the tissue is flooded with nutrients and oxygen, and cell metabolism collapses,” Ferreira explains.
In response to stress, cardiac cells produce large amounts of 4-HNE (4-hydroxy-2-nonenal), a reactive aldehyde that is toxic in excess and destroys essential cellular structures. The mitochondrial enzyme ALDH2 normally rids the organism of accumulated aldehydes—both 4-HNE in stressed cardiac cells and the acetaldehyde resulting from ethanol breakdown in the liver after a bout of drinking.
In previous research, however, Ferreira’s group, in partnership with colleagues at Stanford led by Daria Mochly-Rosen, showed that ALDH2 activity during the process of ischemia and reperfusion was significantly reduced. These findings were published in Science Translational Medicine and Circulation Journal.
“The amount of 4-HNE becomes so large inside the cardiac cells that it ends up attacking the enzyme ALDH2, which should be metabolizing it,” Ferreira said.
“In our new study, we observed that ALDH2 activity in the heart exposed to ethanol before ischemia-reperfusion injury remained equal to that seen in a healthy heart. We believe the stress caused by a moderate dose of ethanol leaves a memory and that the cell learns to keep ALDH2 more active,” added the coordinator of the FAPESP-funded research.
Five groups
Mice were divided into five groups to explore the mechanisms underlying the observed cardioprotective effect. The hearts in the control group suffered no damage and received no treatment or intervention. The hearts in the second group were submitted to ischemia and reperfusion, losing approximately 50 percent of their cells as a result.
In the third group, before inducing the ischemic injury, the researchers exposed the hearts extracted from male mice to ethanol for 10 minutes, at a dose equivalent to two cans of beer or two glasses of wine for an average man. The dose was adjusted according to each animal’s mass.
“We endeavored to follow the recommendation of the World Health Organization (WHO), which is up to one dose per day [18 grams of alcohol] for women and up to two doses per day for men. In the case of mice, it was around 50 millimolar,” Ferreira explained.
The hearts were washed for 10 minutes to remove surplus alcohol, and the flow of oxygen and nutrients was then interrupted, as for group two. An analysis performed approximately one hour after reperfusion showed that only 30 percent of the cells had died. In other words, the damage was reduced by almost 60 percent in comparison with group two. Also, the FAPESP-supported study found that ALDH2 activity was twice as high as in the untreated group and equivalent to the level measured in the control group, which was not submitted to the insult.
In the fourth group, the hearts were treated with ethanol and exposed to a drug that inhibits ALDH2 activity. In this case, the rate of cell death rose from 50 percent to 80 percent, confirming that the protection provided by ethanol does indeed depend on the action of this enzyme.
The fifth and last group consisted of hearts from mice with a mutation in the gene encoding ALDH2 that reduced the enzyme’s activity by almost 80 percent. As Ferreira explained, the mice were genetically modified to simulate this mutation, which is very common among humans of East Asian descent and affects over 500 million people worldwide.
“In this group, when we exposed the hearts to ethanol, the damage caused by ischemia and reperfusion was greater,” he said. “The rate of cell death rose from 50 percent to 70 percent. However, when we treated this group’s hearts with Alda-1, an experimental drug that activates ALDH2, it fell to 35 percent.”
Treatment with Alda-1 was not found to benefit the hearts of mice without the ALDH2 gene mutation when exposed to ethanol. “This suggests that both the experimental drug and alcohol act on the same molecular mechanism to activate ALDH2,” he added.
Alda-1 has completed Phase I clinical trials in the US and is classified as safe for use in healthy humans. In a new phase of trials due to begin soon, it will be administered to patients with heart disease.
Role of DNA
Ferreira drew a parallel between regular consumption of small amounts of alcohol by humans and the results observed in the hearts of mice treated with ethanol in the laboratory.
“However, it all depends on people’s DNA,” he stressed. “The acetaldehyde that results from digesting ethanol may protect most people if a small amount is produced, but it can also maximize the damage done by a heart attack in an individual with the ALDH2 gene mutation. It’s easy to identify these people. After one glass of beer, they get flushed and complain of a headache. Their resistance to alcohol doesn’t improve over time.”
Heart damage may also be exacerbated if a large amount of alcohol is consumed, Ferreira warned, as this results in excessive production of acetaldehyde and makes the cleansing normally performed by ALDH2 much harder.
“The group treated with the ALDH2-inhibiting drug [in which the rate of cell death reached 80 percent] mimicked what happens when a person drinks too heavily. The hard part is establishing the safe dose for each individual. There are many variables that affect alcohol digestion,” Ferreira said.
The researchers at ICB-USP are now trying to understand how the presence of acetaldehyde resulting from the metabolizing of alcohol in heart cells creates the memory that keeps ALDH2 more active. The idea is to develop a drug that mimics the beneficial effect of ethanol without exposing the individual to risks such as chemical dependency.
Source: Read Full Article