Researchers from Queen’s University Belfast have discovered a new way to predict the aggressiveness and future behavior of prostate cancers.
The new method uses images from computed tomography (CT) scans that are routinely collected from all patients. The images are then analyzed by a computer to extract hundreds of features, termed ‘radiomic features,” which have the potential to uncover disease characteristics that fail to be seen by the naked eye.
This technique could complement traditional assessment methods and may help clinicians to make more informed personalized treatment decisions for men with prostate cancer. In the long run, it may reduce or even replace the need for traditional invasive biopsies.
The research has been published in the International Journal of Radiation Oncology, Biology, and Physics and was carried out in collaboration with the Northern Ireland Cancer Centre and Maastricht University.
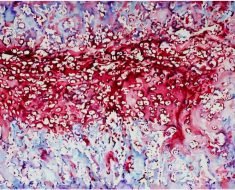
Prostate cancer is one of the most common forms of cancer, but the behavior of an individual cancer is extremely variable. While some tumors metastasize rapidly, others can remain harmlessly localized in the prostate gland for years.
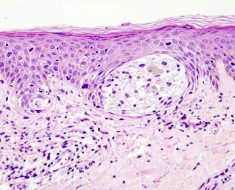
Dr. Suneil Jain, principal investigator from the Centre for Cancer Research & Cell Biology at Queen’s University Belfast, said: “To predict the risk represented by a given tumor, Gleason scores are typically assigned based on how a sample of the tumor appears under the microscope compared with normal prostate tissue. Patients are then classified as low, medium, or high risk depending on their Gleason score, level of prostate specific antigen (PSA) in the blood, and on size of the tumor and whether it has spread to other parts of the body.”
The research team used CT scans for 342 prostate-cancer patients acquired as a routine care prior to radiotherapy treatment. Focusing on the prostate gland, the researchers then extracted and analyzed over 500 radiomic features from each image. These features, along with the Gleason score and risk group classification for each patient, were used to “train” a computer to be able to discriminate between patients in low- and high-risk groups, and between those with low and high Gleason score.
CT-based classification models proved able to discriminate between patients from different Gleason score and risk groups. The system was especially competent at distinguishing between patients in low- and high-risk groups, and between those with low and high Gleason score.
Dr. Sarah Osman, Lead Investigator and Postdoctoral Research Fellow at Queen’s University Belfast and the Belfast Health and Social Care Trust, explained: “This is the first CT-based radiomics investigation for this treatment site and it is showing very promising results. Although the present study will not revolutionize prostate cancer treatment by itself, it shows what could be possible in the future. We are building on collaborations with other institutes to provide datasets to validate our exciting findings and take this discovery forward.”
Professor Philippe Lambin from the Maastricht University and one of the co-inventors of Radiomics added: “Typically, there isn’t a huge amount of quantitative data in radiology reports. With the radiomics revolution, we need to look at medical images not just as pictures, but as quantitative data potentially useful for trials and routine care.”
Professor Ian Young, chief scientific advisor to the Department of Health in Northern Ireland and director of HSC R&D said: “Cancer is a major cause of morbidity and mortality. By supporting research like this, we can ensure that patients have access to the most innovative cancer treatments, and the best preventive strategies can be put in place.”
Dr. Matthew Hobbs, deputy director of research at Prostate Cancer UK said: “We’re delighted to see more results coming out of the Prostate Cancer UK and Movember funded Centre of Excellence.
Source: Read Full Article