At current drug prices, testing all persons entering prison for Hepatitis C, treating those who have at least 12 months remaining in their sentence, and linking individuals with less than 12 months in their sentence to care upon their release would result in improved health outcomes. Published in Clinical Infectious Diseases, researchers found that these approaches provide the best value-for-money compared to not testing or treating any prisoners, or only testing and treating prisoners at high risk of Hepatitis C (HCV). While cost-effective, however, the data also show that these approaches would place a large cost burden on the correctional system.
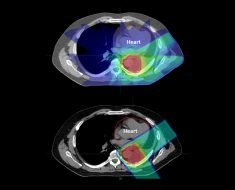
Researchers simulated the lifetime progression of a cohort of prisoners from intake until death, projecting clinical outcomes, cost-effectiveness, and the budgetary impact. They considered different levels of testing (no testing, risk-based testing, routine testing at entry or at release), whether treatment would or would not be provided in prison, and whether or not a patient would be linked to care upon release if he/she were not treated in prison. The “test all, treat all, and linkage to care at release” strategy increased the number of people cured by 23 percent, reduced cirrhosis cases by 54 percent, and increased life expectancy for HCV-infected individuals by two years. It was determined that this strategy was cost-effective when compared to current practice; however, it was associated with an additional annual cost to the department of corrections of $1,440 per prisoner entering the system, a significant burden on health care budgets.
Approximately one third of all U.S. HCV cases pass through the prison system each year, making interventions among incarcerated individuals important in reaching the World Health Organization’s goal of eliminating HCV. Policymakers might understand the importance of controlling HCV rates in prison, but need data like this to inform the costs and outcomes they can expect from a variety of testing and treatment strategies.
“We expected clinical outcomes to improve with widespread testing, treatment, and linkage to care for individuals not treated in prisons, but found it notable that it was also the strategy to most efficiently use limited health resources,” said Sabrina Assoumou, MD, MPH, infectious diseases physician at BMC and the study’s lead author. “Addressing HCV in prisons will require investment from departments of corrections and public health departments, but we hope these findings demonstrate the value of such an investment and will encourage innovations in financing HCV care among this population.”
Source: Read Full Article