Most Australians diagnosed with COVID-19 recover at home, rather than in a quarantine facility or hospital. About 10% have required hospital treatment. However, a handful have had worsening symptoms, did not receive emergency care and died at home.
There appear to have been two factors behind such COVID deaths at home: worry about the perceived costs and risks of seeking official health care; and the sudden onset of complications from a worsening infection.
Here’s what to watch out for when symptoms worsen dramatically at home and when to call an ambulance.
What should I look out for?
As a GP I am asked this question often. Patients naturally want guidance on the signs to look out for so they don’t seek help too late or too early. This is called “safety netting”, and is guided by an understanding of the natural history (prognosis) of a disease and its response to treatment. People also seek advice on worrying symptoms to look out for, and specific information on how and when to seek help.
With COVID-19, the natural course of the infection varies. What starts out with cold and flu-like symptoms can lead to breathing difficulties within five days. Not all patients get symptoms that warrant hospital care. But of those who do go to hospital, this generally occurs around 4-8 days after symptoms start.
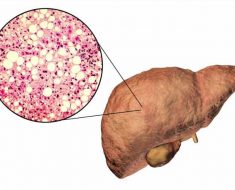
We know COVID-19 affects the lungs as well as multiple organs, leading them to fail. This includes complications such as pneumonia, liver or kidney failure, heart attacks, stroke, blood clots and nerve damage.
This progress to more severe disease happens as the virus triggers release of inflammatory proteins, called cytokines, flooding the bloodstream and attacking organs.
Some symptoms of these COVID complications include:
- shortness of breath
- loss of appetite
- dizziness
- confusion or irritability
- persistent pain or pressure in the chest
- high temperature (above 38℃).
- reduced consciousness (sometimes associated with seizures or strokes)
- cold, clammy or pale and mottled skin.
Not everyone feels ‘short of breath’
The main risk factors that predict progression to severe COVID include: symptoms lasting for more than seven days and a breathing rate over 30 per minute. Faster breathing is to compensate for the less-efficient transfer of oxygen to lung blood vessels, due to inflammation and fluid build-up in the airways.
But how diseases progress is rarely straight forward, making it impossible to give definitive lists of “red flag” symptoms to look out for.
Some COVID patients have “happy” or silent hypoxia. This features low levels of oxygen in the blood but there aren’t the usual signs of respiratory distress normally seen with such low oxygen levels, including feeling “short of breath” and faster breathing.
However, these patients can suddenly deteriorate. Faster and deeper breathing are early warning signs of failing lungs.
What to do
If you’ve already been diagnosed with COVID-19 and are concerned about your symptoms, call the phone number you will have been given by your local public health unit, or your health-care provider.
However, for a sudden deterioration, call an ambulance immediately. Tell the operator you have COVID.
If you’re not sure which applies or you can’t get through on the phone for medical advice immediately, call 000 anyway as operators are trained to triage your call.
Being in hospital if you develop severe COVID, with access to the best monitoring and treatments available, will increase your chance of surviving complications of COVID, and recovering well.
Source: Read Full Article