A fascinating new study, released as a preprint on the medRxiv* server, adds a highly appealing tool to the armory of detection techniques for the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Its validation could allow the early and accurate detection of recent or active infection, which is valuable in tracing contacts and preventing forward transmission of the virus.
.jpg)
Background
With the spread of the SARS-CoV-2 over the inhabited world, causing the coronavirus disease 2019 (COVID-19) pandemic, methods of identifying the prevalence of the infection have been eagerly sought. One such method has been the seroprevalence survey, covering various antibody subsets targeting the viral spike or nucleoprotein antigen.
These antigens appear from 5-7 days after symptoms set in, and the overall detection of immunoglobulin G (IgG) antibodies ranges from 58-74%, and for IgM from 46% to 70%, with a specificity of approximately 99% in both cases. The low sensitivity makes this unsuitable for the diagnosis of early SARS-CoV-2 infections or to distinguish those in the past from recent infections.
Applications of serological testing include contact tracing backward to define the index cases and immediate contacts. Since these are probably negative for the viral ribonucleic acid (RNA) genetic material, or antigen, or both, the reverse transcriptase polymerase chain reaction (RT PCR) test is likely to be negative.
This is especially so in long-term care homes and assisted living facilities, schools and frontline workplaces.
About dimeric IgA
IgA is the most abundant antibody isotype in humans and characterizes the mucosal immune response. In plasma, about 90% of IgA is monomeric, mostly of IgA1 isotype, with 10% being dimeric (dIgA), with two monomers connected through the J chain.
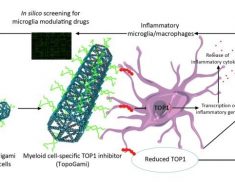
This form of IgA gives rise to secretory IgA (sIgA), which is secreted onto mucosal surfaces, neutralizing pathogens by preventing their entry, binding to effector cells to promote the clearance of the pathogen or toxin, or inhibiting toxin effects. Dimeric IgA binds to the polymeric Ig receptor (pIgR) on epithelial cells, facilitating transport across the mucosal epithelium. At the other end of the cell, the receptor is cleaved, and the sIgA is released, namely, dIgA bound to the secretory component of the pIgR.
Spike-specific IgA has a half-life of 210 days, and thus its detection cannot specify the presence of a recent infection. Plasma dIgA is found only in recent infections.
How was the study conducted?
In this experiment, the researchers designed a novel point of care, lateral flow assay (LFA) that detects dIgA binding to the SARS-CoV-2 spike receptor binding domain (RBD) in plasma.
This was based on dIgA binding to a chimeric form of the pIgR that is extremely specific for the dIgA, followed by immobilization of dIgA-RBD complexes. The pIgR showed no reactivity to monomeric IgA or IgG specific for the same antigen even at 200 or more times the limit of detection for IgA.
The specificity of the test was confirmed by testing it against multiple samples containing pre-pandemic plasma specimens and those from infections confirmed to be other than COVID-19.
Specific dIgA appears early in infection
Using this, they found that the presence of RBD-binding dIgA had 95.5% specificity for recent SARS-CoV-2 infection, while total IgA was only 86% specific. Either plasma or whole blood showed similar positivity levels for both total Ig and dIgA. Thus, the study provided a proof of concept that testing for SARS-CoV-2 dIgA in whole blood could detect anti-RBD total Ig and dIgA.
The dIgA levels began to increase 0-10 days after symptom onset. In about half the patients, it was detectable by five days. It was detectable in all infected participants by the 11th day, with the mean level being approximately 8,800 units. The peak was on days 14-15.
This pioneering study provides the missing link to active or recent SARS-CoV-2 infections, which are not picked up by IgM levels, unlike many other infections. The early appearance of dIgA and its link to sIgA indicates that it is a potent neutralizing antibody against this virus, compared to monomeric IgA.
Conversely, the acute marker of infection, IgM, was found to appear only after day 5, that too in about 40% of patients by day 10. Between days 11-15, it was detected in 92% of subjects. IgG levels were detected in 34% at days 6-10, increasing to 67% between 11-15 days.
The levels of dIgA were moderately associated with IgG levels to the N protein, with all samples becoming positive for the latter by days 14 and 15. IgA antibodies to the S1 subunit of the viral spike protein were correlated with dIgA levels at days 11-15 in all but one case.
What are the implications?
Taken together, these data suggest that dIgA may be an acute phase serological marker of SARS-CoV-2 infection, that dIgA is generated earlier than both IgM and IgG and follows a similar trajectory to IgA early in infection. Unlike total IgA, dIgA levels decline more rapidly in plasma beyond 15 days after symptom onset.”
Anti-S1 IgG antibodies were maintained at steady levels over a longer period, with a half-life of approximately 14 days, two to three times longer than dIgA, with a half-life of approximately 6 days.
IgA is not so helpful as it is found to be present over a much longer period, at stable levels, while dIgA shows a clear trend in titer, being present at detectable levels in 100% of infections with SARS-CoV-2 after 11 days from the onset of symptoms, but clearly declining after 20 days. One patient stands out for the strong dIgA response despite an undetectable IgA response.
Thus SARS-CoV-2-specific dIgA seems to offer great promise as an accurate biomarker of recent SARS-CoV-2 infection when carried out by a rapid point-of-care LFA. The short half-life means it is not useful to detect past infections, but in contrast, the high percentage of detection between 11-35 days, the early phase of infection, shows that it is a unique biomarker for the serological diagnosis of current or recent infection.
The dIgA test performs at its best in the 2nd and 3rd week post symptom onset and a positive result by itself would indicate recent infection.”
The scientists suggest its use in combination with a rapid antigen test, to allow large-scale screening for active or recent infections. It could be used to trace contacts backward to the primary case, establish transmission chains, and minimize the number of people required to isolate to break such chains.
*Important notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Drummer, H. E. et al. (2021). Dimeric IgA is a specific biomarker of recent SARS-CoV-2 infection. medRxiv preprint. doi: https://doi.org/10.1101/2021.06.28.21259671. https://www.medrxiv.org/content/10.1101/2021.06.28.21259671v1.
Posted in: Device / Technology News | Medical Science News | Medical Research News | Disease/Infection News | Healthcare News
Tags: Antibodies, Antibody, Antigen, Assay, Biomarker, Blood, Cell, Coronavirus, Coronavirus Disease COVID-19, Genetic, Immune Response, Immunoglobulin, Pandemic, Pathogen, Polymerase, Polymerase Chain Reaction, Protein, Receptor, Respiratory, Reverse Transcriptase, Ribonucleic Acid, RNA, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Syndrome, Toxin, Virus

Written by
Dr. Liji Thomas
Dr. Liji Thomas is an OB-GYN, who graduated from the Government Medical College, University of Calicut, Kerala, in 2001. Liji practiced as a full-time consultant in obstetrics/gynecology in a private hospital for a few years following her graduation. She has counseled hundreds of patients facing issues from pregnancy-related problems and infertility, and has been in charge of over 2,000 deliveries, striving always to achieve a normal delivery rather than operative.
Source: Read Full Article