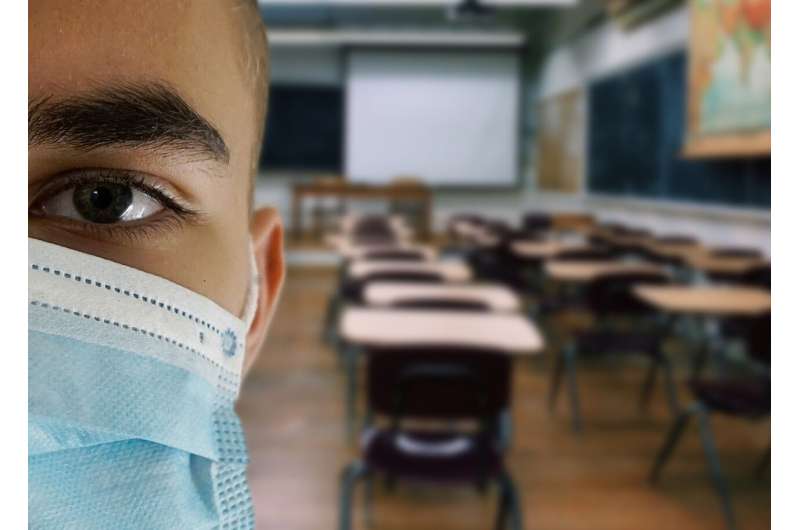
Just when schools were getting ready to reopen for the new school year, cases of COVID-19 started surging in the United States, driven in large part by the more contagious delta variant. School administrators around the country are working to bring students back into the classroom safely, while still providing kids an enriching learning environment.
As an infectious disease epidemiologist at the University of Washington, I have spent the past year and a half working with a group of epidemiologists and health professionals to collect, review and evaluate the scientific evidence about COVID-19 for state and local public health agencies.
Our group concluded that vaccines and masking work well for preventing COVID-19 outbreaks in schools, but other strategies like plexiglass barriers and temperature checks are probably not worth the effort.
What works
A COVID-19 vaccine is the single most important tool for preventing COVID-19 in schools, as well as nearly everywhere else. All the vaccines currently authorized for use in the U.S. have been shown to help prevent infections and protect against moderate and severe disease. Some variants, such as delta, may be more likely to cause breakthrough infections, but vaccinations have shown protection against symptomatic disease caused by delta.
The more people in a school who are vaccinated, the lower the risk of an outbreak in the school and the lower the likelihood that someone will develop severe disease if infections occur. COVID-19 vaccines are currently available to anyone age 12 or older, and it is possible that at least one of the vaccines will be authorized for younger school-age children in the later months of 2021 or early in 2022.
Masks are important, too. Not everyone in a school can be or will choose to be vaccinated, and there is also a risk of breakthrough infections, especially from the delta variant. Masks reduce the risk of an infected person’s spreading the virus and provide some protection for the wearer against becoming infected. During the past academic year, mask-wearing was shown to reduce the spread of COVID-19 in schools. Masks also don’t disrupt the school day in the way that other measures might, such as keeping students in fixed cohorts or shortening the school day for split shifts.
What probably isn’t worth the effort
Other prevention measures have had limited effectiveness in some settings but likely are not worth the cost and effort to implement in most schools.
Plexiglass barriers, common in businesses and other venues, can be expensive and do little to prevent airborne transmission in school environments. In some situations, barriers like desk shields may actually increase the risk of transmission by reducing air circulation.
Daily temperature checks and symptom screening have also not proved to be an efficient way to prevent COVID-19 in public settings. This approach misses asymptomatic cases, which are especially common among children and younger adults. Still, students, teachers and staff should stay home until they have a negative test if they are experiencing symptoms of COVID-19 or have been exposed to someone with COVID-19.
Other policies can reduce transmission but can be disruptive to students, like physical distancing of at least 6 feet or separating students into cohorts that are not permitted to mix. If students are wearing masks, and especially if most are vaccinated, these measures are unlikely to add much more protection. The CDC currently recommends 3-foot spacing in schools when possible and multilayered prevention measures when not possible.
It’s also probably not worth testing everyone on a regular basis. Frequent testing is expensive, and real-world examples and mathematical models indicate that routine asymptomatic testing for COVID-19 in schools provides little additional benefit beyond widespread vaccination and masking. However, the CDC does include some asymptomatic testing in schools as one of the potential components of a layered prevention strategy.
What to do about lunch
When I talk to school administrators about reopening safely, one of the most common questions they ask me is how to run lunchtime, when students are gathered together and cannot always wear masks. Many schools included lunch during the past year without causing COVID-19 outbreaks, which suggests that lunch can be done safely.
There is little direct evidence on the risk of transmission when comparing different approaches to the lunch problem, but there are some basic guiding principles.
Students should wear masks whenever they are not actively eating. As challenging as it is to manage a rambunctious lunchroom, shouting, singing and loud talking spread more virus and should be discouraged, especially without masks. And good ventilation, particularly in spaces where people are eating, is important.
Students also need to keep their distance from one another while they eat. Schools may consider having more lunch periods, having children eat in their classrooms, or using other spaces in the school to reduce crowding.
Risks outside of school
The strongest driver of COVID-19 in children, teachers and families is not school—it’s the level of community transmission.
Given what we currently know, schools can continue to operate in person without widespread transmission linked to schools. When community transmission is high, schools should take extra care to stick to their prevention strategies. But the main way to protect students is to stop the spread of COVID-19 outside of school.
What we still don’t know
It’s not clear how the rise of the delta variant will affect the return to school. People infected with delta tend to spread the virus more than those infected with other strains, and breakthrough infections from this variant can cause large outbreaks when other prevention measures are not in place. Relying on vaccinations alone to control COVID-19 does not seem to be a winning strategy.
More children are becoming infected during the delta variant surge. There have been sharp increases in July and August 2021 in the total number of children identified with infections and hospitalized for COVID-19. But the number of cases in the general population has increased, too. There has only been a modest increase in the proportion of COVID-19 cases in children relative to other age groups, and that could be due to the fact that children are an increasing share of the unvaccinated.
Source: Read Full Article