A new survey by City University of New York School of Public Health researchers and posted to the medRxiv* preprint server suggests the prevalence of severe acute respiratory syndrome coronavirus 2 (SARS‑CoV‑2) among adults in the U.S. during the BA.5 surge was much higher than the official CDC case counts would suggest, with substantial disparities associated with social determinants of health. Therefore, this may cause future inequities in the long-COVID burden.
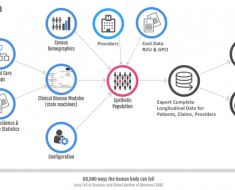
 Study: The prevalence of SARS-CoV-2 infection and long COVID in US adults during the BA.5 surge, June-July 2022. Image Credit: Donkeyworx / Shutterstock
Study: The prevalence of SARS-CoV-2 infection and long COVID in US adults during the BA.5 surge, June-July 2022. Image Credit: Donkeyworx / Shutterstock
Background
The ongoing coronavirus disease 2019 (COVID-19) pandemic of 2020, caused by SARS-CoV-2, has infected over 603 million individuals and accounts for more than 6.48 million global deaths to date. Although the deployment of vaccines aided in limiting the disease, the emergence of newer variants of concern (VOCs) with greater transmissibility and vaccine-escape capability has escalated the disease burden.
These mutants and the waxing and waning course of the pandemic have warranted continuous monitoring of COVID-19 and studies on the short and long-term (long COVID) consequences. Long COVID manifests at least four weeks after SARS-CoV-2 infection; it affects millions of Americans. The Centers for Disease Control and Prevention (CDC) estimates that one in five American adults suffer from long COVID symptoms. The current predominant circulating subvariant in the U.S. is Omicron BA.5.
COVID-19's true disease burden is difficult to track due to the continually evolving virus, the decline in appropriate screening measures, and the increasing use of rapid antigen tests at home. Moreover, the positive tests were not adequately reported as many patients remain undiagnosed while others may not visit a physician or tend to manage the symptoms at home despite a positive test report. Hence, population-based surveys need to be carried out to improve public health mitigation measures.
The study
A population-based survey was conducted in the U.S. to estimate the prevalence of COVID-19, characterize the associated factors of infection, and for testing and the pervasiveness of long COVID among adults with a history of prior SARS-CoV-2 infection.
The survey included 3,042 randomly-selected U.S. adult residents contacted through landlines and mobile phones between June 30 and July 2, 2022. The survey questionnaire enquired about the results of SARS-CoV-2 tests; vis, at-home rapid diagnostic tests, viral PCR, or rapid antigen carried out during the Omicron BA.5 surge in the region – that is, 14 days before the survey.
Results
During this cross-sectional survey, Omicron BA.5 was the predominant variant in the U.S. The findings revealed that 43,993,550 adults in the U.S. had SARS-CoV-2 infection during the study period, of whom most of the adults had COVID-19 positive test results––according to a healthcare service provider, while others were either tested at home or were assumed to be COVID-19 positive based on the SARS-CoV-2 infection criteria.
The SARS-CoV-2 infection prevalence was higher in the 18-24-year age group and more significant in males. In addition, Hispanic adults and individuals of lower socioeconomic and educational status showed a higher preponderance of COVID-19 positivity. The disease also showed regional variations – with more cases in the Western parts of the U.S followed by the Northeastern parts.
Individuals with hybrid immunity had a higher propensity to re-acquire SARS-CoV-2 infection than those with infection-induced immunity. Other groups with – only vaccine-induced protection and SARS-CoV-2 naïve individuals showed a lower prevalence of the infection. Thus, past infection was an important marker of re-infection risk, rather than the vaccination status, during surges. Meanwhile, unvaccinated individuals had a higher prevalence of SARS-CoV-2 infection than those over 65 years. At the same time, individuals with comorbidities had the highest COVID-19 prevalence. All these groups were also predisposed to severe COVID-19 symptoms. Most individuals with either of these vulnerabilities were found to be SARS-CoV-2 positive.
However, less than half of the participants had been tested for COVID-19 during the study period. Individuals between 18-24 years of age were more likely, and those above 55 were less likely to undergo COVID-19 tests. Participants who most often opted for COVID-19 tests were Hispanics, less educated individuals, those employed, people from the Northeastern parts, and those with hybrid immunity and who received booster doses.
Less than one-fourth of the participants with SARS-CoV-2 infection reported long COVID symptoms at least four weeks before the survey. The prevalence of long COVID was higher in the age range of 35-44 years; females; unemployed people; Black non-Hispanics; and people with existing comorbidities. The prevalence of long COVID was lower among people above 65 years of age, males, and those who were uninsured.
The prevalence of long COVID was also higher in females with comorbidities and insured women. An individual's vaccination status did not pose any statistically significant difference in the long COVID prevalence.
Conclusion
The prevalence of SARS-CoV-2 infection in the U.S. during the Omicron BA.5 surge depicts substantial levels of infection circulation – much higher than the official CDC case counts. In addition, all cases of SARS-CoV-2 cases were not registered with the CDC pointing toward disparities in social health determinants. Yet, many people suffer from symptoms of long COVID. Therefore, better disease surveillance by more population-based surveys is warranted to mitigate the pandemic.
*Important notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Qasmieh, S., Robertson, M., Teasdale, C., et al. (2022). The prevalence of SARS-CoV-2 infection and long COVID in U.S. adults during the BA.5 surge, June-July 2022. medRxiv* preprint. Doi: 10.1101/2022.09.04.22279588, https://www.medrxiv.org/content/10.1101/2022.09.04.22279588v1
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: Antigen, Coronavirus, Coronavirus Disease COVID-19, Diagnostic, Healthcare, immunity, Omicron, Pandemic, Public Health, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Syndrome, Vaccine, Virus

Written by
Nidhi Saha
I am a medical content writer and editor. My interests lie in public health awareness and medical communication. I have worked as a clinical dentist and as a consultant research writer in an Indian medical publishing house. It is my constant endeavor is to update knowledge on newer treatment modalities relating to various medical fields. I have also aided in proofreading and publication of manuscripts in accredited medical journals. I like to sketch, read and listen to music in my leisure time.
Source: Read Full Article